Research Article: 2021 Vol: 24 Issue: 1S
An Evaluation of Public Health Schemes in India: A Case Study of Maharashtra State
Gaikar Vilas B, University of Mumbai
Abstract
The significance of health is elaborated in the current research paper on the study of public health schemes in Maharashtra, India. Since it is true that “Health is wealth,” health has been frequently discussed and debated issues in recent years. According to a UNDP survey from 2018, the United States ranks 37th in the world in terms of life expectancy, while Hong Kong ranks fourth. India is ranked 133rd in entire world, with its life expectancy of 69.4 years. “A state of full physical, emotional, and social well-being of the person, not merely the absence of disease or infirmity,” according to the 1948 report by World Health Organization (WHO).
The state is a well-developed health facility that offers comprehensive health services to its citizens, especially in rural areas. The department has increasingly gained control over major diseases such as Guinea worm and small pox. At the same time, leprosy and neonatal tetanus have been eradicated in the province. Since 2011, Maharashtra’s polio immunization programme has resulted in non- identification of polio cases. More than Rs. 3965.57 crores has been invested on public health by the ministry. Introduction, study of literature, research methods, and public health schemes in Maharashtra state, data interpretation, and recommendations are among the parts of the paper.
Keywords
Public Health, Comprehensive Health Services, Health Schemes, Social Wellbeing
JEL Classification
I10, I18, I38, R59
Introduction
Health is a priceless gift from nature to humans, and it is one of the acute fundamental needs that are affected by a number of factors such as food, accommodation, basic sanitation, safe lifestyles, environmental hazards security, and communicable diseases. Health is man’s natural state and birthright, arising from living in compliance with natural laws regulating the body, mind, and environment. Fast access to critical services such as health care is one of the most important aspects of healthy living. However, for someone who is unable to access these resources, it may also mean the difference between life and death. As a result, without sufficient health care services, an important aspect of social sector growth is missing (Vilas, 2017).
Health is a basic human right as well as a global social objective. Health is needed for the fulfillment of basic human needs and the attainment of a higher standard of living. In many developing countries, improving the quality of growth is an essential aim of the development archetype. Better health, education, equitable and expanded work opportunities for everyone, people's intuition that is trustworthy and open, a sustainable and cleaner world, integrity, self-esteem, and life protection, to name a few, are main manifestations of growth quality (Kausar, 2021).
“A state of full physical, emotional, and social well-being of the person, not merely the absence of disease or infirmity,” according to the 1948 report by World Health Organization (WHO). Health care, which means the treatment as well as management of disease at the same time the protection of health through services rendered by medical, dental, pharmaceutical, clinical laboratory sciences, and allied health professions, is a vital sector to improve for a better standard of living. (World Health Organization (WHO) Report 2011-12)
The key theme of healthcare is to provide comprehensive health services, to protect everyone’s physical, social, and mental health, to reduce mortality rates, to improve man’s life expectancy, and to promote social growth in a sustainable manner. The growth of healthcare facilities is affected not just by the facilities themselves, but also by the proper administration and management of health staff. Adequacy, availability, accessibility, affordability, and viability are all attributes of a successful healthcare system.
One of the most hotly debated subjects in recent years has been public health. The adage “Health is wealth” is real. When opposed to their counterparts in other countries, most developed countries face a plethora of health-related issues. According to a UNDP survey from 2018, the United States ranks 37th in the world in terms of life expectancy, while Hong Kong ranks fourth. India is ranked 133rd in the world, with a life expectancy of 69.4 years (UNDP survey 2018).
Maharashtra is one of India’s most progressive states, with an annual growth rate of 7.5 percent. For the fiscal year 2018-19, the Gross State Domestic Product (GSDP) is estimated to be Rs. 26,60,318 Crore. For the 2017-18 fiscal year, the per capita state income is Rs. 1,76,102. The state is a well-developed health facility that offers comprehensive health services to its citizens, especially in rural areas (Govt. of Maharashtra, 2017).
Objectives of the Study
The present research paper has been based on various objectives; these are as follows;
1. To study health services in India.
2. To evaluate health services in Maharashtra.
3. To study Central and State governments expenditure on health schemes.
4. To evaluate expenditure on health schemes in Maharashtra State.
5. To suggest various measures for improvements in health standard in the state.
Hypotheses
The present research on study of public health schemes and expenditure in Maharashtra state has following hypotheses;
1. There has been constant increase in the expenditure by the Central and State government on health schemes.
2. An increase in the public expenditure on the health has improved the life expectancy of the citizen.
3. The public health schemes by the government have benefited to the underprivileged people.
Scope and Limitation of the Study
The current report on public health schemes in Maharashtra involves a review of various public health schemes, as well as state and federal government spending on improving people’s health. The research is limited to only public schemes run by the central and state governments, leaving out the private sector. The study area is constrained by the Maharashtra state’s jurisdiction an analysis has been done on the basis of secondary data.
Introduction, study of literature, research methods, and public health schemes in Maharashtra state, data interpretation, and recommendations are among the parts of the paper.
Review of Literature
The current analysis on Maharashtra’s public health schemes is focused on previous studies and references that have been published in the form of research papers, books, journals, documents, and annual reports. The following are some excerpts from the literature review:
The Prevention and cure are treated as separate inputs into the household health output function by Grossman & Rand (1974). They believe that groups with a low health capital stock depreciation rate demand preventive health care and groups with a high health capital stock depreciation rate need curative health care. This encourages customers to regard prevention and cure as interchangeable terms. Differences in endowed health are magnified in terms of attained survival because a higher endowment of health raises demand for health expenditure. Grossman (1974) if health-care spending raises, the productive potential of the working population and, as a result, the level of income rises, contributing to a decrease in the rate of poverty (Vilas, 2016).
In their research paper, titled “Current Health Scenario in Rural India,” they attempted to objectively analyze India’s current health status, with a particular focus on the large rural population at the dawn of the twenty-first century. They have concentrated on improving the current situation, as well as the issue of rural health on a macro and micro level, in order to ensure good health for the poorest members of society. To address the needs of the rural population, they introduced a paradigm change from the current “Biomedical model” to a “Socio-cultural model” (Ashok, 2002)
He researched “Access to healthcare in the fractured setting of India’s fast increasing agglomerations” at the United Nations Office for the Prevention of Cruelty to Persons. In this essay, the author explored India’s healthcare sectors, healthcare issues in India, and mapped healthcare centres in Pune. The article’s main finding is that rapid urbanization causes gaps in healthcare access (Butsch, 2008).
He looked at “Socio-economic disparity and its effect on healthcare” in the Indian community, as well as the impact on the healthcare system. It aims to recognize the factors that contribute to the challenges of healthcare delivery in an unequal society, as well as their effect on society’s health (Milind, 2004).
“Assessing the availability of Primary health care facilities in Chamarajanagara District using Kernel Density Estimation,” wrote in a joint paper. The authors used Kernel Density Estimation to determine the availability of Primary Health Care Centres in Chamrajanagar district for evaluating population coverage of health services. They estimated accessibility rations such as population to Primary Health Centre and population to health workforce using kernel density estimation. They discover that the health centres are dispersed across the district in an unequal manner. The aim of this article is to further improve various forms of accessibility in order to evaluate population coverage of services (Divya, 2012).
“Rural health issues and solutions around the world.” In this article, the author addresses the major challenges that rural health faces around the world, reviews the issues, and tries to examine the tremendous challenges that are faced in improving the health of people living in rural and remote areas of the world, as well as a particular action plan such as the global initiative on rural health plan. It focused world attention on rural health and marked the beginning of a new era for improving people like doctors, nurses, and other health workers in rural areas around the world to give “Health for all rural people” it marked the beginning of a new era for improving people like doctors, nurses, and other health workers in rural areas around the world to give “Health for all rural people” it focused world attention on rural health and marked the beginning of a new era for improving people like doctors, nurses, and other health workers in rural areas (Strasser 2003).
Research Methodology
The present research on the topic “An evaluation of public health schemes in Maharashtra state: A study” is based on the secondary data collected from various sources like Ministry of health, annual reports by the ministries from both the Central and State government. The collected secondary data has been analyzed by using various statistical tools and techniques such as average, Pearson’s correlation coefficient and so on (Anderson, 1958; Cherian et al., 2021; Cherian et al., 2020; Gupta, 2019).
Public Health Schemes in Maharashtra State
The state’s health department seeks to provide high-quality health care by prioritizing disadvantaged people in numerous federally-sponsored programs that the state has implemented. The department has increasingly gained control over major diseases such as Guinea worm and small pox. At the same time, leprosy and neonatal tetanus have been eradicated in the province. Since 2011, Maharashtra’s polio immunization programme has resulted in no polio cases being identified (Dhawan, 2015).
While national health initiatives such as malaria eradication, leprosy prevention, and blindness control are successfully implemented in the state, the Family Welfare Program remains the core theme of the public health programme. The public health sector is concentrating on the consolidation of infrastructure facilities such as Sub-Centers, Primary Health Centers, and community health care centers in order to provide health services to all parts of the state (Government of India, 2002).
In tribal areas, the state health department has concentrated on mental health care, AIDS prevention, cancer prevention, and special health facilities. During the monsoon season, Malaria, Gastroenteritis, and other water-borne diseases are widespread in tribal districts such as Thane, Nashik, Dhule, Amravati, and Gadchiroli. The Health Department is also in charge of overseeing the medical facilities established under the ESIS. Public health is described as the science of ensuring the protection and improving the health of communities through disease and injury prevention education, policy development, and research. In India, the government has been at the forefront of healthcare growth. Simple to advanced health care services are delivered by federal, private, and voluntary health care facilities.
The goal of public health services is to provide the community with dependable, accountable, sufficient, qualitative, preventive, and curative health care, with an emphasis on maternal and child health. Furthermore, public health facilities are provided with local and cultural diversity in mind, particularly for tribal and rural communities (Government of India, 2002).
To provide comprehensive health services to the people, the GoM has established a three-tier health system. Sub Centres, Primary Health Centres (PHC), and Community Health Centres make up the primary category (CHC). The secondary tier includes sub-district hospitals in rural and semi-urban areas, as well as district-based hospitals. At the tertiary level, there are well-equipped medical colleges and super-specialty hospitals in major cities (Govt. of Maharashtra, 2017) (Table 1).
| Table 1 Various Health Schemes in Maharashtra State and Expenditure (2018-19)(Value in Rs. Crores) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proposed Outlay2017-18 | Revised Estimate2018-19 | Expenditure Up to28 Feb2018 | Budgeted2018-19 | |||||||||
| State | Center | Total | State | Center | Total | State | Center | Total | State | Center | Total | |
| Directorate of General Health Services | 296.06 | 118.54 | 414.60 | 400.07 | 118.80 | 518.87 | 253.41 | 1.84 | 255.25 | 277.10 | 132.92 | 410.02 |
| Family Welfare Program | 68.03 | 768.04 | 836.07 | 68.03 | 768.04 | 836.07 | 147.12 | 530.26 | 677.38 | 130.73 | 849.41 | 980.13 |
| Mahatma Jotiba Phule Jan aarogya Yojana | 473.05 | 0.00 | 473.05 | 1715.11 | 0.00 | 1715.11 | 1208.80 | 0.00 | 1208.80 | 561.50 | 0.00 | 561.50 |
| National Aayush Mission | 11.85 | 23.54 | 35.39 | 20.17 | 47.07 | 67.24 | 0.00 | 18.75 | 18.75 | 11.85 | 21.30 | 33.16 |
| National Health Mission | 651.66 | 1661.16 | 2312.82 | 1273.79 | 2030.49 | 3304.28 | 864.16 | 833.80 | 1697.96 | 753.57 | 1585.51 | 2339.08 |
| Total | 1853.54 | 2719.45 | 4572.99 | 3830.06 | 3112.57 | 6942.63 | 2579.31 | 1386.27 | 3965.57 | 1998.15 | 2591.83 | 4589.97 |
| Source: https://arogya.maharashtra.gov.in/ and authors own calculations | ||||||||||||
Result Details & Calculation
X Values
∑=3858.14
Mean=771.628
∑(X - Mx)2=SSx=1891564.539
Y Values
∑=4323.89
Mean=864.778
∑(Y - My)2=SSy=3177243.353
X and Y Combined
N=5
∑(X - Mx)(Y - My)=2083170.698
R Calculation
r=∑((X - My)(Y - Mx))/ √((SSx)(SSy))
r=2083170.698/ √((1891564.539)(3177243.353))=0.8497
Meta Numerics (cross-check)
r=0.8497
The value of R is 0.8497
This value 0.8497 shows the strong positive correlation, which means that when there is an increase in the budgetary expenditure there is also increase in the actual expenditure of the government to the health expenditures (Table 2).
| Table 2 Various Health Schemes in Maharashtra State and Comparative Expenditure By Central and State Government (2018-19) (Value in Rs. Crores) |
|||
|---|---|---|---|
| Health schemes in Maharashtra | Expenditure Up to28 Feb2018 | ||
| State | Center | Total | |
| Directorate of General Health Services | 253.41 | 1.84 | 255.25 |
| Family Welfare Program | 147.12 | 530.26 | 677.38 |
| Mahatma Jotiba Phule Jan Aarogya Yojana | 1208.80 | 0.00 | 1208.80 |
| National Aayush Mission | 0.00 | 18.75 | 18.75 |
| National Health Mission | 864.16 | 833.80 | 1697.96 |
| Total | 2579.31 | 1386.27 | 3965.57 |
| Source: https://arogya.maharashtra.gov.in/ and Authors own calculation | |||
Explanation
It is clear from the above table that there is significant contribution by the Central Government on the health schemes especially Family Welfare Program (FWP) i.e., Rs. 530.26 Crores and on National Aayush MissionRs. 18.75 Crores at the same time Rs. 833.80 Crores were spent on National Health Mission(NHM).
It has been also interpreted from the table that 53.74 % of total expenditure is headed by the Central Government. The co relation between state expenditure on health and total health expenditure has been measured by the Pearson Correlation Coefficient is as follows:
Result Details & Calculation
X Values
∑=2473.49
Mean=494.698
∑(X - Mx)2=SSx=1070200.312
Y Values
∑=3858.14
Mean=771.628
∑(Y - My)2=SSy=1891564.539
X and Y Combined
N=5
∑(X - Mx)(Y - My)=1184231.46
R Calculation
r=∑((X - My)(Y - Mx))/ √((SSx)(SSy))
r=1184231.46/ √((1070200.312)(1891564.539))=0.8323
Meta Numerics (cross-check)
r=0.8323
The value of R is 0.8323.
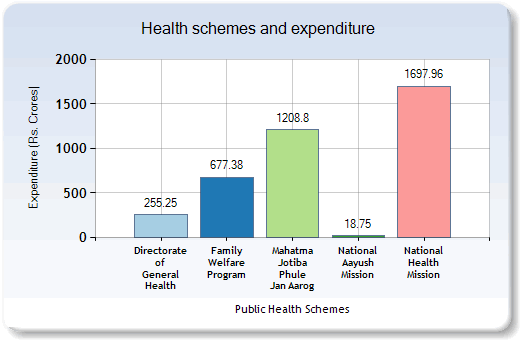
So, according to the Pearson Correlation Coefficient there is a strong positive correlation, which means that state expenditure on health also increases as there is an increase in the total expenditure irrespective of an increase in the expenditure of central government expenditure on health. (Figure 1)
Above Fig. 1 Health Schemes and Expenditure (Rs. Crores) states that on various health schemes the government has made expenditure. (IBEF, 2016)
The Healthcare Services and Schemes in Maharashtra State
There are various schemes and programs for providing health services in the Maharashtra state, these are as follows; (Government of Maharashtra health schemes, accessed from https://arogya.maharashtra.gov.in accessed on, 6th February 2018)
Directorate of Health Services
This agency's primary responsibilities include general medical care, disease prevention, family health, mother and child development, sanitation, nutrition, and medical resource training. According to this departmental survey, the budgeted outlay for fiscal year 2018-19 was Rs. 410.02 crores.
StateBloodTransfusion Council
The State Blood Council was formed in Maharashtra on the 4th of January, 1996, by Supreme Court order. Under the auspices of the Blood Transfusion Council, the State Blood Transfusion Units were formed in the state to ensure an adequate supply of healthy blood and blood products at a fair cost. For the fiscal year 2018-19, the budget for this scheme was Rs. 25.00 crores.
Mahatma Jotiba Phule Jan Arogya Yojana
Mahatma Jyotiba Phule Jan Arogya Yojana initiated and included new beneficiaries, increase in sum assured amount of per family per year, increase in number of empaneled hospitals & additions of new procedures with a motto to give benefits to more and more beneficiaries. The Budgeted Outlay for the year 2018-19 was Rs. 561.50 Crores.
Family Welfare Program
The Maharashtra government is introducing the Family Welfare Program (FWP) in compliance with Indian government guidelines, primarily to achieve population control. The state’s Total Fertility Rate (TFR) has already reached 1.8. For the fiscal year 2018-19, the budgeted outlay was Rs. 980.13 crores.
National Health Mission
National Rural Health Mission is being introduced in the state in compliance with the Central Government’s guidelines. The Mission’s goal is to provide all citizens of the state with safe, affordable, efficient, responsible, and reliable health care. This includes the poor and vulnerable. School health checkups are one of the essential tasks carried out under the NRHM. Strengthening of sub-centers by ASHA and AYUSH. Sickle Cell Disease Control Program, establishing health institutions in accordance with Indian Public Health Standards, telemedicine, geriatric treatment, and other initiatives are underway. For the fiscal year 2018-19, the budgeted outlay was Rs. 2339.08 crores.
National Ayush Mission
During the 12th Plan, the Department of AYUSH, Ministry of Health and Family Welfare, Government of India, launched the National AYUSH Mission (NAM) for implementation across states and union territories. The National AYUSH Mission was initiated by the Indian government with the following goals:
1) Providing cost effective AYUSH Services through upgrading AYUSH Hospitals & dispensaries, & co-location
2) Up gradation of AYUSH educational institutions
3) Up gradation of ASU & H Pharmacies, Drug Testing Laboratories & strengthening of ASUSH drug enforcement mechanism
4) Supporting the cultivation of medicinal plants to provide sustained supply of quality raw-materials. The Budgeted Outlay for 2018-19 is 33.16 Crore.
Aids Control Program
Maharashtra State Aids Control Society and Mumbai Aids Control Society are in charge of implementing the National AIDS Control Program. The focus is entirely on public awareness programs, education, and surveillance of particular populations. Surveillance is carried out by screening blood samples from Sexually Transmitted Disease (STD) clinic patients and women seeking antenatal treatment.
Conclusion and Suggestions
The present research on the topic “An evaluation of public health schemes in Maharashtra state: A study” is based on the secondary data collected from various sources like Ministry of health, annual reports by the ministries from both the Central and State government. The collected secondary data has been analyzed by using various statistical tools and techniques such as average, Pearson’s correlation coefficient and so on. It has been observed that there has been continuous growth in the public expenditure on various health schemes and it has resulted into reduce in health problems of the state. It is seen from the study that only few cities are having the best facilities for health improvements but is needed to provide all the necessary health facilities to all the cities and villages. It is true that ‘India lives in villages’ so the government has to provide proper attention for the betterment of the health services in the rural parts of the country and the state.
Following are some of the Suggestions on the Study
The present research has various suggestions on the basis of data analysis and review of literature and available in the form of; the schemes initiated by the Central government has to be appropriated adopted and implemented by the State of Maharashtra (Vilas, 2017).
The budgetary allocation for the various health schemes by the governments need to be executed and funds to be utilized properly. There is need to provide vide publicity for various health schemes, so that the poor and needy can be benefited. The important activities being implemented under NRHM including School Health checkup. ASHA, AYUSH etc. needed to be properly implemented and monitored. There is need to check an accountability of the health schemes. Government hospitals should be well equipped with the entire necessary infrastructure to deliver health schemes. There is need to have proper implementation of National AYUSH Mission. There is scope for medical tourism in the nation and the State of Maharashtra, so by developing an appropriate infrastructure it may be possible. Mahatma Jyotiba Phule Jan Arogya Yojana in the state of Maharashtra need to be implemented properly and the benefit should reach to the unreached.
Thus, the present research paper on the health schemes in the Maharashtra state has focused on the proper evaluation of the budgetary and actual expenditure on the health schemes in the State of Maharashtra. The paper also suggested some measures to improve the health status in the state in an appropriate manner.
References
- Anderson, T.W. (1958). ‘Introduction to Multivariate Statistical Analysis’. Wiley: New York.
- Ashok, V.P., Somasundaram, K.V., & Goyal, R.C. (2002). “Current health scenario in rural India”. Australia journal of rural health, 10, 129-135.
- Azhar, S. (2015). Impact of liquidity and management efficiency on profitability: An empirical study of selected power distribution utilities in India. Journal of Entrepreneurship, Business and Economics, 3(1), 31-49.
- Ariffin, S.K., Ng, F., & Mohsin, A.M.A. (2021). Examining the influencing factors of consumer purchase intention toward fast food with health concerns as a moderator. Journal of Entrepreneurship, Business and Economics, 9(2), 39-71.
- Butsch, C. (2008). Access to healthcare in the fragmented setting of India's fast-growing agglomerations: A case study of Pune. In Bohle, H.-G. & Warner, K., editors, Megacities. Resilience and Vulnerability. Bonn, United NationsUniversity.https://www.researchgate.net/publication/232290609_Burden_of_direct_and_indirect_costs_of_illness_Empirical_findings_from_slum_settlements_in_Chennai_South_India [accessed January 7 2021].
- Cherian, J., Gaikar, V., Paul, R., & Pech, R. (2021). Corporate culture and its impact on employees’ attitude, performance, productivity, and behavior: An investigative analysis from selected organizations of the United Arab Emirates (UAE).Journal of Open Innovation: Technology, Market, and Complexity,7, 45.
- Cherian, J., Jacob, J., Qureshi, R., & Gaikar, V. (2020). Relationship between entry grades and attrition trends in the context of higher education: Implication for open innovation of education policy.Journal of Open Innovation: Technology, Market, and Complexity,6, 199. https://doi.org/10.3390/joitmc6040199
- Deogaonkar, M. (2004), “Socio-Economic inequality and its effect on healthcare delivery in India: Inequality and healthcare”, Electronic Journal of Sociology.
- Divya, S., Tali, J.A., & Chandrashekara, B. (2012). “A Geographical study of inequality in distribution of public healthcare centers in Hunsur Taluk, Mysuru”. International journal of environmental sciences, 1(4), 294-298.
- Dhawan, A. (2015). Healthcare Outlook India”. Deloitte India, Available [online].
- Gurtoo, A., & Williams, C.C. (2009). Entrepreneurship and the informal sector: Some lessons from India. The International Journal of Entrepreneurship and Innovation, 10(1), 55-62.
- Gaikar, V., Bharat, M.J., Jaywant, B., Mhatre, N.S., Chitra, K., Cheriyan, S., & Caroleena, G.R. (2021). ‘An impact of covid-19 on virtual learning: The innovative study on undergraduate students of Mumbai Metropolitan Region’. Academy of Strategic Management Journal, 20(2), 1-19.
- Gaikar, V.B. (2018). “Can poverty alleviation possible in India? A study of Thane district’ in ‘North Asian International Research Journal of Social Science & Humanities’, 3(6), 12-17
- Gaikar, V.B. (2017). “An evaluation of agricultural marketing in India a study of national agricultural co-operative marketing federation of India Ltd. (NAFED).” In ‘International Journal of Multidisciplinary Research and Development’, 4(5), 244-248.
- Gaikar, V. (2017). An empirical analysis of trends and opportunities in the Indian healthcare services. International Journal of Multidisciplinary Research and Development, 4(5), 249-252. (Accessed on 10th February 2021)
- Gupta S. C. (2019). Fundamentals of Statistics, Himalaya Publishing House Pvt. Ltd., Mumbai
- Government of India (2002). National Health Policy 2002.
- Govt. of Maharashtra (2017). Handbook of basic statistics of Maharashtra
- Government of Maharashtra health schemes, accessed from https://arogya.maharashtra.gov.in accessed on, 6th February 2018.
- Govt. of Maharashtra (2017). Handbook of basic statistics of Maharashtra.
- Grossman, M., & Rand, E. (1974). “Consumer incentive for health services in chronic illnesses,” in S.J. Mush kin (Ed) Consumer Incentives for Healthcare, (Milbank Memorial Fund: New York), 114-151.
- Gaikar, V. (2016). Has a poverty alleviation program successful in Maharashtra? A study of Thane District. International Multidisciplinary Research Journal-Golden Research Thoughts, 6(2), 1-7. IBEF (2016). “Indian Healthcare Industry Analysis”, Sectoral Presentation made by Indian Brand Equity Foundation.
- Korakod, T., Alhassan, A., Bawa, M., Abdul-A.M., Harrisson, S.K.D., & Gaikar, V. (2021). ‘Optimization of the enterprise HR management by using IoT’ Materials today: PROCEEDINGS, July 2021
- Kausar, M., Siddharth, V., & Gupta, S.K. (2021). A study on economic evaluation of an outreach health-care facility in Jhajjar District of Haryana: Service delivery model for increasing access to health care. Indian Journal Public Health, 65, 45-50.
- Narmadha, V., & Anuradha, A. (2021). Socioeconomic, cultural and environmental impact of covid-19 on tourism in India. Journal of Management Information and Decision Sciences, 24(4), 1-9.
- Roger, S. (2003). “Rural health around the world: Challenges and solutions”. Family Practice, 20(4), Oxford University Press, 20, 457–463.
- Salamzadeh, A. (2020). What constitutes a theoretical contribution? Journal of Organizational Culture, Communications and Conflict, 24(1), 1-2.
- Tariq, M.U., & Abonamah, A.A. (2021). Covid-19 impact on student's mental and social health: Strategy exploration. Academy of Strategic Management Journal, 20, 1-11.
- UNDP survey 2018
- World Health Organization (WHO) Report 2011-12.