Research Article: 2021 Vol: 24 Issue: 1S
Socioeconomic Status Determines Psychological Stress Differences between Older Adults Living In Rural and Rurban Areas during the Post-Coronavirus Disease 2019 Pandemic Era: A Geographic Information System-Based Spatial Analysis
Kukiat Tudpor, Mahasarakham University
Worawit Jitsukka, Mahasarakham University
Chalard Chantarsombat, North Eastern University
Kemika Sombateyotha, Mahasarakham University
Ranee Wongkongdech, Mahasarakham University
Adisorn Wongkongdech, Mahasarakham University
Thanyarat Chaiyakarm, Mahasarakham University
Songkramchai Leethongdeesakul, Mahasarakham University
Nutchanun Kamonroek, Ubon Ratchathani Provincial Health Office
Narongsakdi Kuboonya-aragsa, Department of Labour Protection and Welfare
Krissanachai Kimchai, Northeasthern Regional Center for Primary Health Care Development
Niruwan Turnbull, Mahasarakham University
Keywords
Older Person, Psychological Stress, Geographic Information System, Rurban Area, COVID-19
Abstract
Psychological stress is a process of behavioral and physiological responses to internal and environmental changes. Older persons are group of people of difficulty in adaptation to such changes due to their physical and social limitations. Pandemics of other infectious diseases had different impacts on psychological stress levels depending on their socio-demographic and geographical variations. This present study was aimed to investigate effects of the coronavirus disease 2019 (COVID-19) pandemic on psychological stress levels in older persons living in rural area (Baan Waai) and rurban area (Khamrieng, the area with diffusion of urban and rural activities) in Maha Sarakham province, Thailand. Spatial distribution of psychological stress and socio-demographic data were collected using Global Positioning System (GPS) and were mapped together using the Geographic Information System (GIS) program. Results depicted that the older persons living in the rurban area had a higher psychological stress level. The psychological stress levels were predicted by occupational and economic statuses, especially in the rurban area due to its predominant dependency on trading products and services. In conclusion, living in rural area with job and adequate income were relieving factors of psychological stress in the older persons during the post-COVID-19 pandemic period.
Introduction
As average human life span is increasing, number of elderly population is also growing. An aging society is defined as a society with more than 7% of the population aged 65 or older; a population with more than 14% is an aged society, and a population with more than 20% is defined as a super aging society (Lee et al., 2018). According to a report of an Office of the National Economic and Social Development Council (NESDC), Thailand is becoming a full-fledged aged society in 2021 as number of elderly population is rising to 13.1 million or 18.7 percent of the total population (Khamken, 2021). This is a challenging issue for older people as they confront multiple age-related changes such as degeneration of tissues and organs, sensitivity pollution and environmental stressors (Nigam et al., 2012; Simoni et al., 2015). Lack of adaptability and resilience to these changes can lead to stress-related physical and mental health problems (Zapater-Fajari et al., 2021).
Impacts of the coronavirus disease 2019 (COVID-19) pandemic globally are prominent. It enormously influences economic, social, political, and healthcare systems in many countries (Jazieh & Kozlakidis, 2020). While social isolation, social distancing, state and home quarantine, and community containment measures were immediately applied, people may experience fear of the consequences of being infected with a potentially lethal virus, loneliness, boredom, and anger during emergency lockdown (Carvalho et al., 2020; Hopman et al., 2020). Personal perception of infectious disease outbreak can effectuate psychological stress (Wu et al., 2009). According to the report of World Bank, economic growth of Thailand was expected to shrink by 5%, taking more than two years to return to pre-COVID-19 Gross Domestic Product (GDP) output levels (Kongrukgreatiyos, 2020). The economic shock related to COVID-19 has adversely affected employment, income, and poverty. Associated with both income loss and self-quarantine, it has been recently reported that psychological stress increased among 42.6% of participants living in urban area of Bangkok, Thailand (Pongutta et al., 2021). The extent of this problem on psychological stress and mental health in elderly population in rural areas of Thailand has not been elucidated.
Mental health is a global public health problem. The World Health Organization (WHO), defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” (Organization, 2004). Therefore, it can be implied that stress is one of the key determinants of individual’s mental health. It has been widely reported that psychological stress is a risk factor for mental health problems (e.g., depression and anxiety) and physical health problems (e.g., stroke and heart disease) (Ryder & Cohen, 2021). Etiology of psychological stress is multifactorial encompassing physical health status, economic status, social relationship, living environment, and stressful events (Ahnquist et al., 2012; Zautra et al., 2005). It has been reported that people living in rural areas with green natural scene were more resilient to psychological stress (Mennis et al., 2018). Meanwhile, people in urbanized city were more stressful compared to those living in rural areas (Dhingra et al., 2009). Situated in the Northeastern region of Thailand, Maha Sarakham province consists of 13 districts with rural-urban disparity (Hong et al., 2020). As aforementioned, older adults have to adapt to challenging stressful situation during COVID-19 pandemic, this present study was aimed to investigate psychological stress distribution in this group of population using a geographic information system. Geographic disparity of psychological stress levels and predicting factors in rural and rurban areas were also determined.
Material and Methods
Research Design and Participants
This present descriptive cross-sectional study was performed in older adults living in Baan Waai subdistrict (rural area, n=1210) and Khamrieng subdistrict (rurban area, n=627), Maha Sarakham, Thailand. It was the part of the project “Development of Mobile Application of Database of Older Persons Using Geographic Information System (GIS) to Detect and Analyze Risks of Chronic Diseases, Quality of Life, and Mental Illness by Village Health Volunteers in 7th Regional Health Office Territory” funded by the Office of the National Digital Economy and Society Commission, Ministry of Digital Economy and Society. All procedures have been conducted in accordance with the Declaration of Helsinki and approved by the Ethical Review Committee for Human Research, Maha Sarakham Provincial Public Health Office (No.6/2564). Written informed consent forms were obtained from all participants. Inclusion criteria were age ≥ 60 years old and household registered in Baan Waai or Khamrieng subdistricts with informed consent. The older adults not physically present during the study were excluded.
Data Collection Tools
The tools for data collection in this study consisted of 3 parts. First, socio-demographic data (gender, age, marital status, living arrangement, educational level, occupational status, activities of daily living (ADL) level, present illness, drinking status, and smoking status). The age 80 years old was used as a cut-off point because of critical changes in levels of sex hormone (dehydroepiandrosterone), muscle mass, physical strength recovery capability(Yiallouris et al., 2019). The Thai version of Barthel ADL index assessment tool developed by the Ministry of Public Health, Thailand was used to evaluate participants’ functional ability (Jantapo & Kusoom, 2021). The standard tool consists of a 10-item questionnaire asking about ADL with the total score of 0 to 20. Its score ranges were classified as independent (12-20) and dependent (0-11) groups. In the present study, the latter two groups were further grouped into the dependent group. Secondly, a 24-item psychological stress questionnaire. Each item was rated on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3= neither agree nor disagree, 4 = agree, and 5 = strongly agree). Possible total score (24-120) was further divided into 4 levels of psychological stress (24-48 = mild, 49-72 = moderate, 73-96 = high, and 97-120 = severe). The tool was constructed and approved for content validity by 3 experts in nursing, psychiatry, and public health. The content validity has been confirmed by index of item-objective congruence (IOC). Only the items with IOC scores ≥ 0.5 were qualified for the questionnaires. The items with Cronbach’s ≥ 0.7 were acceptable and used in the questionnaire. The socio-demographic and psychological stress data were collected by local Village Health Volunteers (VHV) using online questionnaires on a mobile phone. Locations of the participants were collected using the global positioning system (GPS) and were mapped together with the psychological stress levels using the geographic information system (GIS) program. The geographic coordinate system used in this study was the World Geodetic System 1984, Universal Transverse Mercator coordinate system (EPSG:32648 WGS 84/UTM Zone 48N). All data collection process was performed from April to July 2021.
Statistical Analyses
Continuous data are expressed as mean and standard deviation. Normality of sample data was tested by the Kolmogorov–Smirnov test. Categorical data are expressed as frequency and percentage. The statistical analyses consisted of two steps: univariate and multivariate analyses. For the univariate analysis, association between the psychological stress levels and the socio-demographic variables were evaluated with compared using Fisher’s exact test. The results showed that there was minimal multicollinearity among the socio-demographic variables. For the multivariate analysis, multivariate ordinal logistic regression was performed. The psychological stress levels were treated as the dependent variable. The socio-demographic variables proven significant at the univariate analysis were entered as independent variables in the generalized linear regression models to gain more power in investigating the effect of risk factors than the conventional logistic regression models using SPSS software version 18 (Armstrong & Sloan, 1989; Mathew et al., 2021).
Results
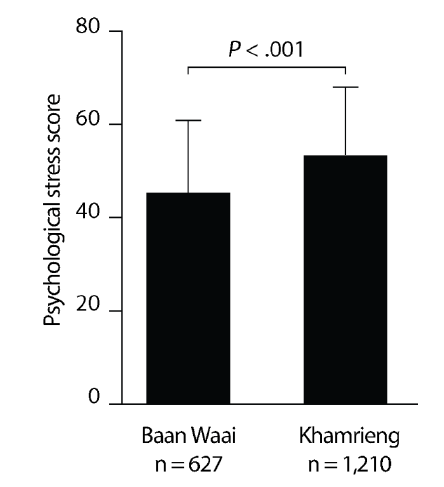
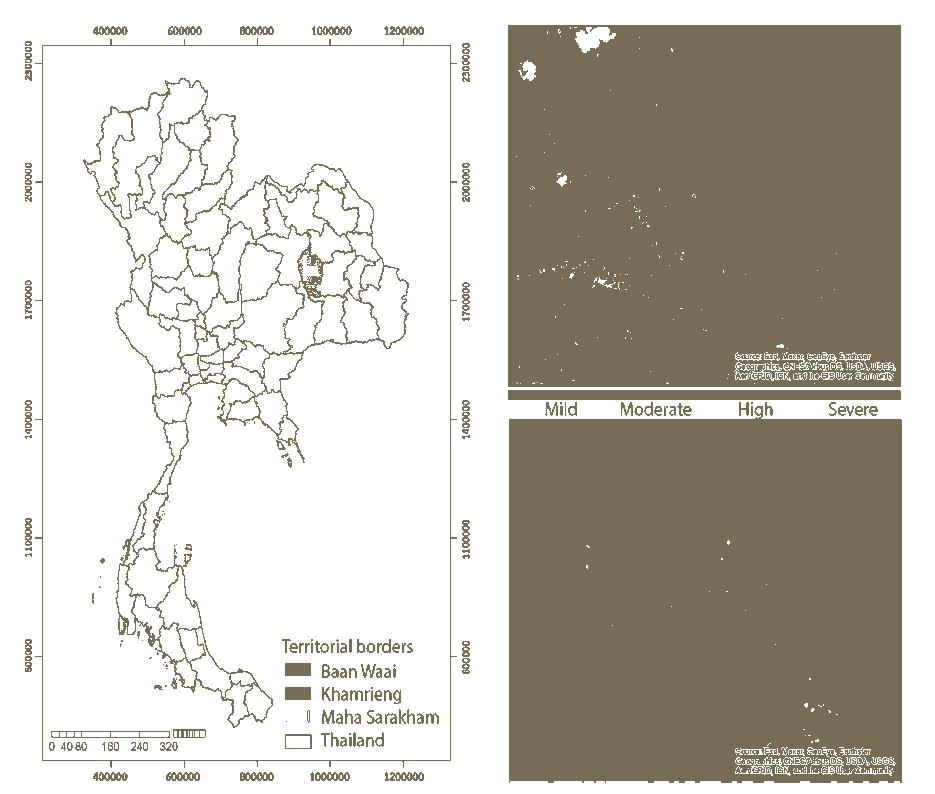
The socio-demographic data of 1,837 older adults from rural (Baan Waai, n = 1,210) and rurban (Khamrieng, n =627) areas are shown in Table 1. Majority of the participants were female with mean age less than 80 years old, being married, living with family, and having at primary school level of education. Most of them were still working, having inadequate income for living. Only 42 participants were in the dependent level of ADL. Approximately 1/3 had ≥ 1 underlying disease of hypertension, diabetes mellitus, and musculoskeletal diseases. Only approximately 10% were drinking alcohol or smoking. The psychological stress scores collected during the post-COVID-19 pandemic era in the last 6 months are shown in Table 2. Results showed that the psychological stress scores in the older adults living in Baan Waai and Khamrieng areas were 44.99±16.18 and 52.94±16.21, respectively. Mean score comparison by independent t-test showed a significant difference between the two groups (P<0.001, Figure 1). Geographic distribution of the psychological levels is illustrated in Figure 2.
Figure 1: Comparison of Psychological Stress Scores (Mean±Sd) Between Rural (Baan Waai) and Rurban (Khamrieng) Areas
Figure 2: Geographical Distribution of Psychological Stress Levels in Community-Dwelling Older Adults in Rural (Baan Waai, Red Border) and Rurban (Khamrieng, Blue Border) Areas
| Table 1 Socio-Demographic Characteristics of Participants (N=1,837) |
||||
|---|---|---|---|---|
| Characteristics | Category | Baan Waai Area n (%) | Khamrieng Area n (%) | P-value |
| Gender | Male | 528 (43.6) | 242 (38.6) | 0.041* |
| Female | 682 (56.4) | 385 (61.4) | ||
| Age | 60-79 | 1061 (87.7) | 561 (89.5) | 0.146 |
| ≥ 80 | 149 (12.3) | 66 (10.5) | ||
| Marital status | Married | 757 (62.6) | 358 (57.1) | 0.024* |
| Single (widowed/divorced/separate) | 453 (37.4) | 269 (42.9) | ||
| Living arrangement | Living with family | 1149 (95.0) | 593 (94.6) | 0.740 |
| Living alone | 61 (5.0) | 34 (5.4) | ||
| Educational level | Higher than primary school | 45 (3.7) | 56 (8.9) | <0.001* |
| Primary school | 1165 (96.3) | 571 (91.1) | ||
| Occupational status | Working | 915 (75.6) | 463 (73.8) | 0.426 |
| Not working | 295 (24.4) | 164 (26.2) | ||
| Economic status | Enough income for living | 553 (45.7) | 230 (36.7) | <0.001* |
| Not enough income for living | 657 (54.3) | 397 (63.3) | ||
| ADL level | Independent | 1175 (97.1) | 620 (97.1) | 0.020* |
| Dependent | 35 (2.9) | 7 (2.9) | ||
| Present illness | No underlying disease | 827 (68.3) | 380 (60.6) | 0.001* |
| ≥ 1 underlying disease | 383 (31.7) | 247 (39.4) | ||
| Drinking status | Non-alcohol drinker | 1036 (85.6) | 563 (89.8) | 0.013* |
| Alcohol drinker | 174 (14.4) | 64 (10.2) | ||
| Smoking status | Non-smoker | 1065 (88.0) | 575 (91.7) | 0.017* |
| Smoker | 145 (12.0) | 52 (8.3) | ||
| Table 2 Psychological Stress Scores During The Post-Covid-19 Pandemic Era in the Last 6 Months (N=1,837) |
|||||
|---|---|---|---|---|---|
| No. | Item description | Psychological stress score | |||
| Baan Waai (n = 1,210) | Khamrieng (n = 627) | ||||
| Mean | SD | Mean | SD | ||
| 1 | I have been afraid of death. | 1.84 | 1.10 | 2.52 | 1.30 |
| 2 | I have been afraid of severe illness. | 2.25 | 1.29 | 2.72 | 1.16 |
| 3 | I have been afraid of being burden of my children and family. | 2.32 | 1.24 | 2.63 | 1.25 |
| 4 | My family members have had conflicts over financial issues and household affairs. | 1.67 | 0.81 | 2.07 | 1.10 |
| 5 | I have felt like I am in “competition” or being compared with others. | 1.61 | 0.79 | 2.03 | 0.98 |
| 6 | I have worried about air, light, noise or water pollution, or even exposure to poisonous substances. | 2.08 | 1.08 | 2.45 | 1.13 |
| 7 | I have been in frustration, fear, and despair of COVID-19 pandemic situation. | 2.33 | 1.15 | 2.81 | 1.20 |
| 8 | I have felt sleepless or frequently have sleep startle. | 1.89 | 0.85 | 2.27 | 0.97 |
| 9 | I have had pain on my back, neck, shoulder, or occipital area. | 2.03 | 0.95 | 2.22 | 0.96 |
| 10 | I have had one-side headache or dizziness. | 1.70 | 0.85 | 1.99 | 0.91 |
| 11 | I have experienced reduced appetite. | 1.81 | 0.87 | 2.15 | 0.94 |
| 12 | I have had frequent urination during night-time sleep. | 1.87 | 0.85 | 2.17 | 0.95 |
| 13 | I have had feeling of discomfort, shortness of breath, or frustration. | 1.63 | 0.81 | 1.89 | 0.91 |
| 14 | I have had feeling of grief or loneliness. | 1.57 | 0.84 | 1.86 | 0.98 |
| 15 | I have felt that I have no enough money for living. | 2.16 | 1.16 | 2.13 | 1.08 |
| 16 | I have had tension or pain in muscle. | 2.01 | 0.95 | 2.05 | 0.88 |
| 17 | I have had frequent feeling of anger or irritation. | 1.70 | 0.86 | 2.19 | 1.35 |
| 18 | I have had headache from stress. | 1.69 | 0.83 | 2.03 | 1.21 |
| 19 | I have felt of confusion, loss of focus, or forgetfulness. | 1.98 | 0.94 | 2.30 | 1.31 |
| 20 | I have had a temporary memory loss. | 2.04 | 0.94 | 2.24 | 1.05 |
| 21 | I have had a migraine. | 1.58 | 0.81 | 1.83 | 0.91 |
| 22 | I have felt tired or faint. | 1.75 | 0.86 | 2.14 | 0.98 |
| 23 | I have had feeling of lack of self-control. | 1.96 | 0.93 | 2.34 | 1.05 |
| 24 | I have felt bored, not doing anything, and wishing to stay alone. | 1.51 | 0.77 | 1.92 | 1.02 |
| Total | 44.99 | 16.18 | 52.94 | 16.21 | |
Furthermore, relationship between the psychological stress levels and socio-demographic characteristics of participants were analyzed by the Fisher’s exact test (Table 3). Results revealed that the psychological stress levels were associated with the locations of living, occupational status, and economic status (P<0.001). In addition, multivariate ordinal logistic regression analysis of independent predictors for psychological stress levels using the generalized linear regression models. Based on the data shown in Table 4, location of living significantly predicted the likelihood of the older adults to have a higher level of psychological stress at P<0.05. The older adults living in Khamrieng area were 2.327 times more likely to have a higher level of psychological stress than those living in Baan Waai area. Similarly, occupational and economic statuses were also the predictors of the psychological stress levels. The older adults without jobs and inadequate income for living were 1.300 and 1.849 times more likely to have a higher level of psychological stress than those with jobs and adequate income.
| Table 3 Relationship Between Psychological Stress Levels and Socio-Demographic Characteristics of Participants |
||||||
|---|---|---|---|---|---|---|
| Characteristic | Psychological stress level | |||||
| Mild n (%) | Moderate n (%) | High n (%) | Severe n (%) | Total n (%) | P- value | |
| Living in Baan Waai area | 790 (65.3) | 330 (27.3) | 89 (7.4) | 1 (0.1) | 1210(100) | |
| Living in Khamrieng area | 261 (41.6) | 291 (46.4) | 69 (11.0) | 6 (1.0) | 627 (100) | <0.001* |
| Male | 456 (59.2) | 247 (32.1) | 64 (8.3) | 3 (0.4) | 770 (100) | |
| Female | 595 (55.8) | 374 (35.1) | 94 (8.8) | 4 (0.4) | 1067 (100) | 0.524 |
| Age 60-79 | 939 (57.9) | 536 (33.0) | 141 (8.7) | 6 (0.4) | 1622 (100) | |
| Age ≥ 80 | 112 (52.1) | 85 (39.5) | 17 (7.9) | 1 (0.5) | 215 (100) | 0.237 |
| Married | 657 (58.9) | 357 (32.0) | 99 (8.9) | 2 (0.2) | 1115 (100) | |
| Single (widowed/divorced/separate) | 394 (54.6) | 264 (36.6) | 59 (8.2) | 5 (0.7) | 722 (100) | 0.059 |
| Living with family | 1,000 (57.4) | 588 (33.8) | 147 (8.4) | 7 (0.4) | 1742 (100) | |
| Living alone | 51 (53.7) | 33 (34.7) | 11 (11.6) | 0 (0.0) | 95 (100) | 0.637 |
| Higher than primary school | 57 (56.4) | 36 (35.6) | 8 (7.9) | 0 (0.0) | 101 (100) | |
| Primary school | 994 (57.3) | 585 (33.7) | 150 (8.6) | 7 (0.4) | 1736 (100) | 0.950 |
| Working | 826 (59.9) | 425 (30.8) | 122 (8.9) | 5 (0.4) | 1378 (100) | |
| Not working | 225 (49.0) | 196 (42.7) | 36 (7.8) | 2 (0.4) | 459 (100) | <0.001* |
| Sufficient income for living | 531 (67.8) | 193 (24.6) | 55 (7.0) | 4 (0.5) | 783 (100) | |
| Insufficient income for living | 520 (49.3) | 428 (40.6) | 103 (9.8) | 3 (0.3) | 1054 (100) | <0.001* |
| Independent level of ADL | 1,032 (57.5) | 602 (33.5) | 154 (8.6) | 7 (0.4) | 1,795 (100) | |
| Dependent level of ADL | 19 (45.2) | 19 (45.2) | 4 (9.5) | 0 (0.0) | 42 (100) | 0.348 |
| No underlying disease | 694 (57.5) | 416 (34.5) | 94 (7.8) | 3 (0.2) | 1,207 (100) | |
| ≥ 1 underlying disease | 357 (56.7) | 205 (32.5) | 64 (10.2) | 4 (0.6) | 630 (100) | 0.174 |
| Non-alcohol drinker | 918 (57.4) | 542 (33.9) | 134 (8.4) | 5 (0.3) | 1,599 (100) | |
| Alcohol drinker | 133 (55.9) | 79 (33.2) | 24 (10.1) | 2 (0.8) | 238 (100) | 0.393 |
| Non-smoker | 946 (57.7) | 554 (33.8) | 133 (8.1) | 7 (0.4) | 1,604 (100) | |
| Smoker | 105 (53.3) | 67 (34.0) | 25 (12.7) | 0 (0.0) | 197 (100) | 0.160 |
| Table 4 Multivariate Ordinal Logistic Regression Analysis of Independent Predictors for Psychological Stress Levels |
||||||
|---|---|---|---|---|---|---|
| Dependent variable | Independent predictors | n (%) | B | OR | 95% CI [lower-upper] | P -value |
| Psychological stress | Living area | |||||
| Baan Waai | 1210 (65.9) | Ref | ||||
| Khamrieng | 627 (34.1) | 0.845 | 2.327 | [1.922-2.818] | <0.001* | |
| Occupation status | ||||||
| Working | 1378 (75.0) | Ref | ||||
| Not working | 459 (25.0) | 0.262 | 1..300 | [1.055-1.603] | 0.014* | |
| Economic status | Ref | |||||
| Sufficient income for living | 783 (42.6) | |||||
| Insufficient income for living | 1054 (57.4) | 0.615 | 1.849 | [1.524-2.244] | <0.001* | |
Discussion
This present study shows the different distribution of psychological stress levels of the older adults living in rural and rurban areas during the post-COVID-19 pandemic era. This disparity is associated with socioeconomic statuses of the older adults. Our conclusion is based on the following findings: 1) the psychological stress score in the older adults living in Baan Waai (rural) area was in a mild level, whereas Khamrieng (rurban) area was in a moderate level, and 2) the older adults without jobs and inadequate income for living were more likely to have a higher level of psychological stress than those with jobs and adequate income.
Mental health is a foundation for well-being and effective functioning for every life of an individual and eventually brings about healthy community (Lahtinen et al., 1999). Being able to cope with stress of life is a key element of healthy mentality (Organization, 2004). From the environment–organism transaction perspective, psychological stress is product of the progressing personal transactions with stressors (environmental or internal perturbations) (Monroe & Cummins, 2015). Severe or chronic psychological stress can lead to behavioral or physiological distress, a negative process of failure to return to homeostasis, which might turn into mental illness (Council, 2008). Therefore, early recognition and management of risk factors for perceived psychological stress are pivotal steps to mental health promotion strategic planning.
Levels of psychological stress increase with an advancing age due to deteriorating health and decline in social relationship (Borson et al., 2001). This present study points out that occurrence of COVID-19 are in close relationship with psychological stress, especially in the rurban area. According to previous studies, Prevalence of Psychological Stress and Posttraumatic Stress Disorders (PTSD) among South Korean and Hong Kong people during outbreaks of Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) significantly increased in the pandemic regions (Lee et al., 2007; Shin et al., 2019). Recently, it has been estimated that an impact of COVID-19 pandemic on psychological stress among Korean people was 1.5 times higher than those who experience MERS (Lee et al., 2020). A study in Nepalese people showed that the influences of COVID-19 pandemic on psychological distress in age group > 45 years old were higher than in the younger age group (Shrestha et al., 2020). They also reported that females and people with post-secondary education had higher risk of developing distress as compared to males and the others with secondary education or lower. In contrast, there are predictive significance of gender and educational levels on psychological stress levels in the present study. As opposed to these findings, this present study signifies the differences in occupational and economic statuses are the predictors of psychological stress levels as shown in the multivariate ordinal logistic regression results. However, the adequate income in the rural area seems to be a solely predicative factor for its relatively low level of psychological stress in comparison to the rurban area as shown in the chi-square analysis results. This might be explained by due to predominant dependency on trading products and services in the rurban area.
Nevertheless, our study also lacks of evident information pertaining to natural and landscape environments. According to literature, Khamrieng is an urbanizing area with high growing rate of infrastructure construction as it is the place where Mahasarakham University is situated in (Chaisantaow et al., 2021). Parts of the land in the neighborhood were transformed from farms to real states because of an increasing number of population and demand in residency, particularly in Khamrieng neighborhoods (Abreu-Vilomar, 2013). It has been reported that people living in a green area have lower psychological stress level (Mennis et al., 2018). Based data from the Global Forest Watch in Maha Sarakham as of 2010, the top 5 regions represent 57% of all tree cover (www.globalforestwatch.org). The data also showed that Wapi Pathum (including Baan Waai) had the most tree cover at 2.25 kilohectare (kha) whereas Kantharawichai (including Khamrieng) was 1.36 ha. From 2001 to 2020, Maha Sarakham lost 141 ha of tree cover, equivalent to a 7.5% decrease in tree cover since 2000 and 67.7 kiloton of CO₂ equivalent emissions. Thus, it can be implied that less green in the urbanizing Khamrieng area might result in higher psychological stress level in older people.
In conclusion, this present study illustrates that the older adults living in rurban area have higher levels of psychological stress compared to those living in the rural areas during the post-COVID-19 pandemic era. This higher psychological stress level is predicted by no occupation and inadequate income of the older adults. These finding should be taken into account by the decision makers in strategic planning as a model to improve mental health of population in the areas.
Acknowledgement
We are appreciative of the financial support by the Office of the National Digital Economy and Society Commission, Ministry of Digital Economy and Society, Thailand. *Corresponding author: Niruwan Turnbull, Mahasarakham University, Thailand, Email: niruwan.o@msu.ac.th.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abreu Vilomar, D. (2013). Sustainable Planning Practices in Maha Sarakham University: A Green Campus for a Learning Community University of Cincinnati].
- Ahnquist, J., Wamala, S.P., & Lindstrom, M. (2012). Social determinants of health--a question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc Sci Med, 74(6), 930-939. https://doi.org/10.1016/j.socscimed.2011.11.026
- Armstrong, B.G., & Sloan, M. (1989). Ordinal regression models for epidemiologic data. American Journal of Epidemiol, 129(1), 191-204.
- Borson, S., Bartels, S.J., Colenda, C.C., Gottlieb, G.L., & Meyers, B. (2001). Geriatric mental health services research: Strategic plan for an aging population: Report of the health services work group of the American association for geriatric psychiatry. The American Journal of Geriatric Psychiatry, 9(3), 191-204.
- Carvalho, P.M.M., Moreira, M.M., de Oliveira, M.N.A., Landim, J.M.M., & Neto, M.L.R. (2020). The psychiatric impact of the novel coronavirus outbreak. Psychiatry Res, 286, 112902. https://doi.org/10.1016/j.psychres.2020.112902
- Chaisantaow, S., Boonserm, W., & Sookngam, K. (2021). The promotion of solid waste management of the dormitories in Khamriang Subdistrict Kantharawichai District, MahaSarakham Province of Thailand. Annals of the Romanian Society for Cell Biology, 25(6), 13213-13225.
- Council, N.R. (2008). Recognition and alleviation of distress in laboratory animals. National Academies Press.
- Dhingra, S.S., Strine, T.W., Holt, J.B., Berry, J.T., & Mokdad, A.H. (2009). Rural-urban variations in psychological distress: findings from the Behavioral Risk Factor Surveillance System, 2007. International Journal Public Health, 54(1), 16-22.
- Hong, V., Iwamoto, S.K., Goto, R., Young, S., Chomduangthip, S., Weeranakin, N., & Nishi, A. (2020). Socio-demographic determinants of motorcycle speeding in Maha Sarakham, Thailand. PLoS One, 15(12), e0243930. https://doi.org/10.1371/journal.pone.0243930
- Hopman, J., Allegranzi, B., & Mehtar, S. (2020). Managing COVID-19 in Low- and Middle-Income Countries. JAMA, 323(16), 1549-1550. https://doi.org/10.1001/jama.2020.4169
- Jantapo, A., & Kusoom, W. (2021). Lifestyle and Cultural Factors Related to Longevity Among Older Adults in the Northeast of Thailand. Journal of Transcultural Nursing, 32(3), 248-255. https://doi.org/10.1177/1043659620921225
- Jazieh, A.R., & Kozlakidis, Z. (2020). Healthcare Transformation in the Post-Coronavirus Pandemic Era. Front Med (Lausanne), 7, 429. https://doi.org/10.3389/fmed.2020.00429
- Khamken, P.W. (2021). Sufficiency Economy Philosophy Towards Poverty Eradication in Thailand. Psychology and Education Journal, 58(1), 1406-1411.
- Kongrukgreatiyos, K. (2020). Major Impact from COVID-19 to Thailand’s Economy, Vulnerable Households, Firms.
- Lahtinen, E., Lehtinen, V., Riikonen, E., & Ahonen, J. (1999). Framework for promoting mental health in Europe.
- Lee, A.M., Wong, J.G., McAlonan, G.M., Cheung, V., Cheung, C., Sham, P.C., Chu, C.-M., Wong, P.-C., Tsang, K.W., & Chua, S.E. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry, 52(4), 233-240.
- Lee, K., Jeong, G.C., & Yim, J. (2020). Consideration of the Psychological and Mental Health of the Elderly during COVID-19: A Theoretical Review. Int J Environ Res Public Health, 17(21). https://doi.org/10.3390/ijerph17218098
- Lee, S.B., Oh, J.H., Park, J.H., Choi, S.P., & Wee, J.H. (2018). Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clinical and Experimental Emergency Medicine, 5(4), 249-255. https://doi.org/10.15441/ceem.17.261
- Mathew, A.C., Siby, E., Tom, A., & Kumar, R.S. (2021). Applications of proportional odds ordinal logistic regression models and continuation ratio models in examining the association of physical inactivity with erectile dysfunction among type 2 diabetic patients. Phys Act Nutr, 25(1), 30-34. https://doi.org/10.20463/pan.2021.0005
- Mennis, J., Mason, M., & Ambrus, A. (2018). Urban greenspace is associated with reduced psychological stress among adolescents: A Geographic Ecological Momentary Assessment (GEMA) Analysis of Activity Space. Landsc Urban Plan, 174, 1-9.
- Monroe, S.M., & Cummins, L.F. (2015). Stress: psychological perspectives.
- Nigam, Y., Knight, J., Bhattacharya, S., & Bayer, A. (2012). Physiological changes associated with aging and immobility. Journal of Aging Research, 2012, 468469.
- Organization, W.H. (2004). Promoting mental health: Concepts, emerging evidence, practice: Summary report. World Health Organization.
- Pongutta, S., Kantamaturapoj, K., Phakdeesettakun, K., & Phonsuk, P. (2021). The social impact of the COVID-19 outbreak on urban slums and the response of civil society organisations: A case study in Bangkok, Thailand. Heliyon, e07161.
- Ryder, A.L., & Cohen, B.E. (2021). Evidence for depression and anxiety as risk factors for heart disease and stroke: implications for primary care. Fam Pract, 38(3), 365-367.
- Shin, J., Park, H.Y., Kim, J.L., Lee, J.J., Lee, H., Lee, S.H., & Shin, H.-S. (2019). Psychiatric morbidity of survivors one year after the outbreak of Middle East respiratory syndrome in Korea, 2015. Journal of Korean Neuropsychiatric Association, 58(3), 245-251.
- Shrestha, D.B., Thapa, B.B., Katuwal, N., Shrestha, B., Pant, C., Basnet, B., Mandal, P., Gurung, A., Agrawal, A., & Rouniyar, R. (2020). Psychological distress in Nepalese residents during COVID-19 pandemic: a community level survey. BMC psychiatry, 20(1), 1-8.
- Simoni, M., Baldacci, S., Maio, S., Cerrai, S., Sarno, G., & Viegi, G. (2015). Adverse effects of outdoor pollution in the elderly. Journal of Thoracic Disease, 7(1), 34-45.
- Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., Liu, X., Fuller, C.J., Susser, E., Lu, J., & Hoven, C.W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. The Canadian Journal of Psychiatry, 54(5), 302-311.
- Yiallouris, A., Tsioutis, C., Agapidaki, E., Zafeiri, M., Agouridis, A.P., Ntourakis, D., & Johnson, E.O. (2019). Adrenal aging and its implications on stress responsiveness in humans. Front Endocrinol (Lausanne), 10, 54. https://doi.org/10.3389/fendo.2019.00054
- Zapater-Fajari, M., Crespo-Sanmiguel, I., Pulopulos, M.M., Hidalgo, V., & Salvador, A. (2021). Resilience and Psychobiological Response to Stress in Older People: The Mediating Role of Coping Strategies. Front Aging Neuroscience, 13, 632141.
- Zautra, A.J., Affleck, G.G., Tennen, H., Reich, J.W., & Davis, M.C. (2005). Dynamic approaches to emotions and stress in everyday life: Bolger and Zuckerman reloaded with positive as well as negative affects. Journal of Personality, 73(6), 1511-1538.