Research Article: 2021 Vol: 25 Issue: 2
Kotter's change model in higher education: transforming siloed education to a culture of interprofessionalism.
Jan Odiaga, Rush University
Mary Jo Guglielmo, Rush University
Cathy Catrambone, Rush University
Theresa Gierlowski, Rush University
Chris Bruti, Rush University
Lynette Richter, Rush University
Joanne Miller, Rush University
Abstract
Culture transformation of an academic medical center, with its “siloed” education and hierarchal structure, is a difficult and slow process. The application of Kotter’s accelerated (XLR8) business change model transformed a siloed academic organization’s culture to one of interprofessionalism. Pressed to effect rapid and sustainable change in an academic medical center, the strategies from the XLR8 model were applied to the hierarchal culture. All the accelerators of the XLR8 model were consciously applied to the change process. Institutional cultural change was validated when: development of an Interprofessional Education (IPE) curriculum was chosen and approved as a quality improvement initiative for accreditation by the Higher Learning Commission; leadership (President and Provosts) funded an office of Interprofessional Education including faculty and support personnel work effort resulting in a year-long IPE course; IPE included in University vision, mission, and strategic plan; unification of four colleges; designated time reserved for IPE; IPE required for graduation, and appears on student transcripts. Kotter’s accelerated model of change is an effective method to remove barriers to educational cultural change. Using Kotter’s change theory model as an infrastructure for change, a large Midwest academic medical center advanced the culture of interprofessionalism, via the development of an IPE curriculum embedded within the University. Kotter’s business model was successfully implemented in a hierarchal academic medical center and other educational institutions with similar cultural structures would likely have success using this change strategy, if the change agents have a clear and deep understanding of the organizational culture. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Keywords
Kotter’s XLR8 Model, Interprofessional Education, Change Model, Culture Change, Health Care Education, Change Theory.
Introduction
Institutions of higher education are faced with a plethora of factors that require institutions to rethink their culture and practices. Demographic changes, financial pressures, technological advancements and now a pandemic, all are catalysts for academic cultural change (Kezar & Eckel, 2002). Yet, in academic medical centers (AMC), the hierarchal structure and “siloed” education culture makes change both difficult and slow. Shifting the culture of “siloed” education (limited interaction between students of different professions) and clinical practice to one of interprofessional education (IPE) and interprofessional collaborative practice is not a new concept. The Institute of Medicine (IOM) in 2001, published “To Err is Human: Building a Safe Health System” which brought attention to medical errors as the leading cause of death in America. Interprofessional communication in the clinical setting was identified as a solution to reduce medical errors, improve patient safety and quality of care IOM (Kohn, Corrigan, & Donaldson). The IOM authored a second white paper, “Health Professions Education: A Bridge to Quality” as an educational solution to improve health care (Greiner & Knebel, 2003). According to this report, health professionals need to learn how to be skilled members of interprofessional teams, communicate effectively, and understand each other’s roles in order to prevent errors thus improving the quality of care. As a result of these landmark papers, health care and educational reforms have been the main driving forces of change. Educational health care reform is guided by accreditation bodies as a form of quality control. They ensure that institutions satisfy the required educational standards across the continuum, starting at the very foundation of health care professional education, into and through care delivery. Although these two systems are different, they have a common goal: create an alignment between educational learning outcomes and health care to improve health care systems.
The educational challenge becomes how to develop a culture of interprofessionalism within a siloed, hierarchal setting, where health professional students not only learn from, with and about each other (WHO, 2010) but have a competency based education-an educational approach to circular design that has an outcomes approach (Frank et al., 2010). In 2011, Interprofessional Education Collaborative (IPEC) an expert panel of health professional educators wrote “Core competencies for interprofessional collaborative practice”. The IPEC core domains, described as competencies, are learned behaviors that are essential for students to prepare for team-based care, while providing patient-centered care. The specific IPEC domains include teams and teamwork, interprofessional communication, values and ethics, and roles and responsibilities. These domains describe the interprofessional competency-based education required of students to become effective interprofessional team members. In 2016, the IPEC expert panel updated the report to include population health and community in the competencies (Interprofessional Education Collaborative, 2016).
In 2014, two transformational campaigns at our AMC collided and provided the catalyst for the “Big Opportunity”. The University was developing a new strategic plan and preparing for reaccreditation through the Higher Learning Commission (HLC). Interprofessional Education (IPE) became integral to the strategic plan and was chosen as our HLC quality improvement project for accreditation. In review of the change management literature, Kotter’s accelerate (XLR8) business model was chosen to bring life to the new IPE strategic initiative Julion et al. (2019) This model was chosen because of its positive, proactive approach for hierarchal, siloed educational institutions to facilitate rapid change in the culture of health care education.
Kotter’s Model of Change
John Kotter, professor at Harvard’s School of Business, created two models of change management. Both were designed for businesses to competitively adapt to their environment. Kotter’s original model (1996) for change was hierarchal and required a stepped approach until a tipping point for change occurred. Sang et al. (2020) applied Kotter’s 1996 model to facilitate change in higher education. Sang’s application of Kotter’s stepped model in a higher education environment stalled due to multiple barriers. The barriers included dynamic changes in faculty, educational practices, faculty autonomy and their lack of involvement in the process. The hierarchical style of Kotter’s 1996 model, combined with its stepped and linear approach, did not match the university culture.
Kotter (2012) redesigned his change management model due to the rapid change driven by technology and later refined the model to accelerate and optimize its efficiency to keep businesses competitive (2014). His refined model called Accelerate (XLR8) increases the rate and success of change in traditional hierarchal organizations (Kotter, 2014). He describes the action of change as the interactions between Dual Operating Systems; one side is hierarchal and the other a self-created network that interacts at multiple touch points, spontaneously and simultaneously throughout the organization (Bradt & Leverage, 2014).
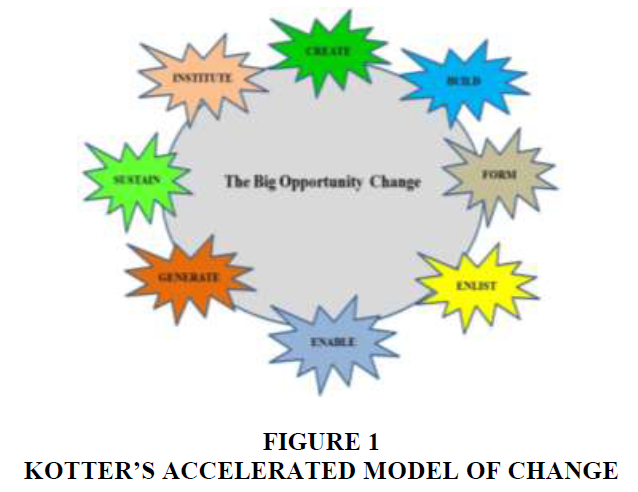
Kotter’s XLR8 model takes advantages of opportunities as they arise in a non-sequential manner. The “Big Opportunity” is the center of Kotter’s theory, defined as the motivator or the nucleus of for change. Circling around the “Big Opportunity”, which is the core of change, there are eight energetic bodies described by Kotter as “accelerators”. Various segments of the organizational structure interact with the accelerators, like atoms circling around the nucleus. The accelerators describe the bold action steps of change leaders, not typically identified in the hierarchy. Action steps are created by the accelerators. They interact with the organizational hierarchy in a nonlinear fashion, at different points and times, to produce change Kang et al. (2020). The resulting effects of the accelerators influence one another through feedback loops, a form of communications which is essential for evaluation and sustainment of the “Big Opportunity” (Bradt & Leverage, 2014; Kotter, 2014).
Although Kotter’s XLR8 change model is not commonly used in education, its use of clear imagery and its concurrent application of accelerators are effective transformation tools for an educational culture. Figure 1 is based on John Kotter's 8-Step Process.
Implementation and Results
Create a Sense of Urgency “Creating a sense of urgency” (Bradt & Leverage, 2014; Kotter, 2014) is identified at the core of cultural change. Kotter refers to this as the “Big Opportunity” in which to engage the entire organization. Creating a sense of urgency involves helping organizational leaders understand why the changes are needed and requires supporting evidence to develop a shared vision. Without developing a shared vision, that employees are willing to support, change will likely fail (Christensen et al., 2014). Strategies used to create a sense of urgency regarding IPE within the University included:
1. Accreditation bodies for health care education added IPE as one of the standards for competency-based education
2. Interprofessional education chosen as the AMC quality improvement initiative for the HLC accreditation
3. Start-up resources to pilot IPE initiative obtained through a three-year grant from Health Resources & Services Administration HRSA-13-186, (Interprofessional Education-Pediatrics through Aging (IPEPA). A curricular gap analysis of over 450 syllabi from all 4 colleges in the university identified the lack of IPE integration into the curricula
4. Results of IPE gap analysis communicated to Leadership, Deans and Curriculum Committees
5. Exit student survey responses from students-initiated grass roots indicated support for IPE.
Build a Coalition
“Building a coalition to guide change” (Bradt & Leverage, 2014; Kotter, 2014) requires passion and involvement from new change leaders and key stakeholders. Top down models for change is often counterproductive and do not convince employees that change is worth their effort (D’Eon, 2013). The coalition team convinces people that change is necessary and persuades others to remove barriers and adopt new practices (Barrow et al., 2020). The Coalition leads the change and is not prescriptive. The team itself is fluid. Strategies used to build a coalition and link it to the hierarchal organizational structure were:
1. IPE curriculum committee formed, comprised of IPE champions from each of the colleges within the AMC
2. Stakeholders identified as President, Provost, Academic Affairs, Student Life, Deans, Curriculum Committees, Registrar’s Office, Department of Marketing and Communication, and Program Directors
3. Regular IPE communications meetings created to inform and update stakeholders
4. Additional IPE champions identified and attended University strategic planning meetings.
Form a Vision for Change “Forming a vision for change” (Bradt & Leverage, 2014; Kotter, 2014) helps accelerate the change process. The vision and mission of our AMC is driven by the strategic plan, which confirms initiatives and endorses the change as an expected outcome of the university. Making the vision a shared common goal amongst stakeholders is essential to achieve the cultural change. For the cultural transformation to become fully embedded the following actions took place:
1. Interprofessional Education included in the University’s vision, mission, and strategic plan
2. Development of a university wide IPE course selected as a quality improvement initiative for accreditation by the HLC
3. IPE course received approval by University Curriculum Committee and Leadership (President, Provosts, and Deans)
4. IPE course became a requirement for graduation and appears as a pass/no pass on student transcripts
5. IPE accounting unit funded the work effort for 15 faculty and support personnel to develop the new IPE course.
Enlist a volunteer army
“Enlisting a volunteer army” (Bradt & Leverage, 2014; Kotter, 2014) facilitates communication of the vision and creates a powerful message of change. Success results from communicating the message at every opportunity in a variety of settings. Communication strategies employed by the IPE team were:
1. Leadership (N=28) and faculty (N=301) from 39 professions attended 17 IP workshops; 13 of these workshops were Lunch and Learns supported by the Office of Continuing Education (N=147)
2. Students (N=1188) from the four colleges volunteered to pilot initial IPE online learning and experiential workshops
3. IPE Curriculum Committee collaborated internally with students and other AMC committees 4. Marketing and website developers enlisted.
Enable Action
“Enabling action” (Bradt & Leverage, 2014; Kotter, 2014) is necessary to remove barriers to change. Common barriers to implementing an IPE course include navigating schedules and space constraints between participating programs, designing course content, and developing faculty knowledge and skills related to IPE and collaborative practice. Actions used included:
1. University Curriculum Committee accepted definitions for IPE, Interprofessional Collaborative Practice and the IPE course syllabus as university standards
2. Faculty development workshops discussed strategies to increase knowledge and overcome barriers
3. Approval of the IPE two-semester course to be listed on students’ transcripts as Pass/No Pass
4. Calendars unified across all four colleges with a designated day and time for IPE course
5. University invested in a Collaborative Learning Hub, an active learning space to house interprofessional, experiential student workshops based on the IPEC competencies.
Generate Short Term Wins
“Generate and celebrate short term wins” (Bradt & Leverage, 2014; Kotter, 2014) is necessary to maintain stakeholders commitment. Faculty and student “buy in” creates a grass roots movement which fuels cultural change. Providing positive feedback to IPE volunteers peaks interest and participation in IPE workshops. Activities to maintain commitment included:
1. Additional funding sources received to support IPE workshops and events provided by student life and deans of colleges.
2. IPE Curriculum Committee established with regular weekly meetings
3. Regular meetings held with University leadership, Deans to share IPE progress
4. Annual luncheon held with Program directors to communicate IPE results
5. IPE abstracts accepted at national conferences
6. Website developed to add interprofessional education
7. IPE success stories published for university newsletters.
Sustain Acceleration
“Sustain acceleration” (Bradt & Leverage, 2014; Kotter, 2014) recognizes that sustainability is not a finite process. It reinforces the changes as the new cultural norms. Continual evaluation of student learning outcomes and qualitative student responses to IPE course continues to ignite cultural change. Establishing polices and a structure to support the change is necessary for sustainability (Farkas, 2013). Efforts to sustain the momentum included:
1. IPE curriculum committee participated in continue strategic plan development.
2. IPE course listed in the university course catalog.
3. IPE course required for first year, on-campus students with automatic batch registration of first year students.
4. Data from IPE course pre and post student surveys evaluated to modify didactic content and delivery methods.
Institute Change
“Institute change” (Bradt & Leverage, 2014; Kotter, 2014) is the final step to the change process. The transformation needs to be continually evaluated and refreshed to remain meaningful to the leadership, stake holders and students, and responsive to the changing educational environment. Transforming the siloed educational culture to one of interprofessionalism was advanced and supported by the institution. This transformation was anchored in the AMC by:
1. IPE became part of the University DNA – included in website, documentation, mission vision, and student participation is expected across the University
2. Office of Interprofessional Education created in the University
3. Enrollment in the IPE 502 course continues to grow since its inception in Fall of 2016 The 2019-20 academic years included 17 professional programs, two intercollegiate relationships, and 695 students.
4. Achievement of student learning outcomes and plans for improvement of IPE course communicated with all stakeholders.
Conclusion
Pushed by the current pandemic, technology and an array of factors, change has never happened faster. In response to the rapid rate of change, educators are challenged to prepare health professional students for the future needs of society. Yet, changing an education culture is no simple task. It requires a large-scale effort to change minds and behaviors. Driven by new health education accreditation standards, IPEC guidelines, and health care reform, AMCs have been tasked with creating a culture of interprofessionalism within their traditionally siloed educational system. Given the pressures to change health care education, we adapted John Kotter’s XLR8 business model to facilitate rapid cultural shift in our hierarchical institution to an interprofessional learning environment. This transformation required working together with open-minded groups who were committed to the “Big Opportunity”. Approaching change spontaneously and simultaneously from all points felt chaotic but provided a process for quick feedback and evaluation from a variety of viewpoints and created an open environment for change. The cultural shift described began from a platform of siloed education and progressed to one of interprofessionalism. Change began at our AMC with a bottom-up, grass roots movement and within three years IPE became an educational standard. The transformational cultural shift resulted in the effective use of resources, improved communication, and increased cooperation throughout the institution. This transformation sparked an innovative educational environment reflecting the mission and vision of the institution’s strategic plan. Kotter’s model would likely have success at other educational institutions with similar cultural structures and change agents who understand the organizational culture and vision. According to Choi (2011) most initiatives for change fail due to the implementation processes not the vision. The fluid nature of Kotter’s model with its multiple, synchronous accelerators have been proven to be an effective framework to drive change. Kotter’s XLR8 business model is nimble by nature and design and has proven to be an effective framework for sustainable change in a higher education institution.
References
- Bradt, G., & Leverage. (2014). Leverage John Kotter's 'Dual Operating System' to accelerate change in large organizations. Forbes. Retrieved from https://www.forbes.com/sites/georgebradt/2014/05/14/leverage-johnkotters-dual-operating-system-to-accelerate-change-in-large-organizations.
- Barrow, J., Annamaraju, P., & Toney-Butler, T. (2020). Change Management. StatPearls Publishing. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK459380.
- Choi, M. (2011). Employees' attitudes toward organizational change: A literature review. Human Resource Management, 50(4), 479-500.
- Christensen, C., Marx, M., & Stevenson, H.H. (2006). The tools of cooperation and change. Harvard Business Review, 84(10), 72-80.
- D'Eon, M. (2013). The challenges of educational change: cultural and psychological inertia. Canadian Medical Education Journal, 4(2), e1-e3.
- Farkas, M. (2013). Building and sustaining a culture of assessment: best practices for change leadership. Reference Services Review, 41(1), 13-31.
- Frank, J., Snell, L., Cate, O., Holmboe, E, Carraccio, C., Swing, S, Harris, P., Glasgow, N., Campbell, C., Dath, D., Harden, R., Iobst, W., Long, D.M., Mungroo, R., Richardson, D., Sherbino, J., Silver, I., Taber. S., Talbot, M., & Harris, K. (2010). Competency-based medical education: Theory to practice. Medical Teacher. 32, 638-45.
- Greiner, A.C., & Knebel. (2003). Committee on the Health Professions Education Summit. Health Professions Education: A bridge to quality.
- Interprofessional Education Collaborative. (2016). Core Competencies for Interprofessional Collaborative Practice.
- Julion, W., Reed, M., Bounds, D.T., Cothran, F., Gamboa, C., & Sumo, J. (2019). A group think tank as a discourse coalition to promote minority nursing faculty retention. Nursing Outlook, 67(5), 586-595.
- Kang, S. P., Chen, Y., Svihla, V., Gallup, A., Ferris, K. & Datye, A.B. (2020). Guiding change in higher education: An emergent, iterative application of Kotter’s change model. Studies in Higher Education.
- Kezar, A., & Eckel, P. (2002). The effect of institutional culture on change strategies in higher education. The Journal of Higher Education, 73(4), 435-460.
- Kohn, L.T., & Corrigan, J., Donaldson, (Eds.). (2020). To Err Is Human Building a Safer Health System. National Academy Press.
- Kotter, J.P. (1996). Leading change. Harvard Business Review Press.
- Kotter, J.P. (2012). Leading change. Harvard Business Review Press.
- Kotter, J.P. (2014). Accelerate: Building strategic agility for a faster moving world. Harvard Business Review Press.
- World Health Organization. (2010). Framework for action on interprofessional education and collaborative practice.