Research Article: 2020 Vol: 23 Issue: 3
Mediation and Mediation in Bioethics in Medical Sphere
Volodymyr I. Bobryk, F.G. Burchak Scientific-Research Institute of Private Law and Business of National Academy of Law Sciences of Ukraine
Svitlana S. Bychkova, National Academy of Internal Affairs
Maryna S. Briukhovetska, Poltava University of Economics and Trade
Liudmyla V. Panova, Taras Shevchenko National University of Kyiv
Vitalii M. Makhinchuk, F.G. Burchak Scientific-Research Institute of Private Law and Business of National Academy of Law Sciences of Ukraine
Abstract
Purpose: The article is to identify the possibility of avoiding conflicts between health care providers and patients through mediation and mediation in bioethics. The Subject of the Study: The subject is the study is the features of mediation and mediation in bioethics on the example of some foreign countries. Methodology: The study used general scientific and special methods of legal science. Thus, the analysis and synthesis method as well as the logical methods were used to formulate a holistic view on mediation and bioethics, as well as to examine their features and peculiarities. The logical-semantic method helped to establish the meaning of the concepts of “mediation”, “bioethics”, “and mediation in bioethics”. The comparative and legal method was applied when analyzing the relevant legislation of Ukraine and some European States regulating the issue under consideration, as well as the views of the scholars on this scientific problem. The historical and legal method was useful in studying the history of the establishment of the term “bioethics”. Using the normative-dogmatic method, the content of regulations of domestic and foreign legislation governing the investigated issue was analyzed. The statistical and legal method was applied to study quantitative indicators and statistics of patients’ complaints about the actions of healthcare providers. The Results of the Study: As the result of the study it was proved that mediation makes it possible not to bring conflict in public (as in the case of justice), but to solve it in private. The advantages of mediation as a way of resolving medical conflicts were identified. Mediation in bioethics, in turn, helps patients or their family members to make difficult choices of appropriate treatment methods. The problems, which can prevent the application of mediation and mediation in bioethics in the medical sphere, were determined. Practical Implications: The necessity to introduce mediation in bioethics in Ukraine, which has been practiced in other countries for a long time, was proved. Value/Originality: The studied dynamic indicators of the number of complaints demonstrate the level of patient protection and inviolability of their rights in Ukraine. This requires standardizing the method of analyzing and interpreting patients’ complaints, as well as introducing mediation, which is characterized as a voluntary process whereby a mediator, who has no interest in the dispute, facilitates communication between the patient and the healthcare provider and helps to resolve their conflict peacefully.
Keywords
Mediation, Bioethics, Medical Sphere, Dynamic Indicators, Patients’ Complaints.
Introduction
The legislation of any State guarantees the patients, who suffer from medical errors or other violations by healthcare professionals, that their rights and interests will be protected in court. Sadly, it is usually long and complicated process in Ukraine, while Ukrainians are suing doctors with increasing frequency. Mediation can be an alternative to judicial dispute resolution, which is a new phenomenon in Ukraine. The institutions of mediation and mediation in bioethics are perhaps the most promising areas, given the trusting nature of the patient-doctor relationship.
The definition of the term “bioethics” was proposed by the American oncologist Potter (1971). He devoted a whole book to this topic called “Bioethics–the bridge to the future”. Potter called bioethics an interdisciplinary ethical doctrine that integrates all cultures and extends the meaning of the word “humanity”. In turn, Saperov (2012) defined bioethics as a moral attitude to all living beings.
The patient’s representative receives his or her “powers” as a result of prior consent between them or in accordance with the procedure established by law in bioethical mediation. In such cases, the person’s ability to represent the patient’s interests is understandable, but problem arises in the case, in which the pre-agreement between the representative and the patient has not previously been made or the representative has some unlawful interest in the matter.
Mediation in bioethics and mediation have the following features: confidentiality, independence, voluntariness, justice, respect of the patient, autonomy of the will, humaneness and others.
Material and Methods
Research methods are chosen based on the object, subject, and purpose of the study. The study used general scientific and special methods of legal science. Thus, the analysis and synthesis method as well as the logical method were used to formulate a holistic view on mediation and bioethics, as well as to examine their features and peculiarities. The logical-semantic method helped to establish the meaning of the concepts of “mediation”, “bioethics”, “and mediation in bioethics”. The comparative and legal method was applied when analyzing the relevant legislation of Ukraine and some other European States regulating the issue under consideration, as well as the views of the scholars on this scientific problem. The historical and legal method was useful in studying the history of the establishment of the term “bioethics”. Using the normative-dogmatic method, the content of regulations of domestic and foreign legislation governing the investigated issue was analyzed. The statistical and legal method was applied to study quantitative indicators and statistics of patients’ complaints about the actions of healthcare providers. The legal modeling method was used applied to draw conclusions and to develop proposals for improving legislative regulation of mediation and bioethics in Ukraine.
The materials studied are the laws and regulations of Ukraine and some foreign countries governing the issues, related to the institutions of mediation and bioethics, scientific works of domestic and foreign scientists on the problems under investigation. Besides, quantitative and statistical indicators of patients’ complaints about the actions of healthcare providers for the period of 2014–2019 were used.
Results
In the broad sphere of bioethics, which is a modern model of medical ethics, the principle of humanity as a respect for human life, which is typical for medical relations at all stages of their existence, is complemented by the aspect of autonomy of the individual, which is realized in medicine by independent decision regarding one’s health.
In turn, autonomy both in bioethics and mediation can include such aspects as respecting the patient’s personality, providing truthful information to the patient, choice of alternatives, making independent decisions, and collaborating (Saperov, 2012).
In addition to the above, the following problems may prevent the application of mediation and mediation in bioethics in the medical sphere: lack of professional training of mediators, lack of the system of guarantees of their independence, lack of information among medical professionals and patients, lack of legal regulation. As a result, the mediation and mediation procedure itself remain uncertain.
In our opinion, it is of the utmost importance to provide the relevant medical institutions with specialists who will have proper education, practical skills, which meet the standards and principles of accreditation of mediators (Chashyna, 2015). Besides, it might be needed to enlist the persons, who work in the medical sphere for a long time, have considerable knowledge of medicine, bioethics, and health care legislation.
The responsibility of informing each patient of the possibility of using mediation should rest with the family physician. Besides, informational lectures and training should be provided for physicians and other healthcare providers to enhance their knowledge and skills in the area of mediation regardless of the ownership of health facility.
It is possible to carry out the activity of mediator on a professional basis both by an individual mediator and by an organization (legal entity) that carries out activities to ensure the conduct of the mediation procedure.
Discussion
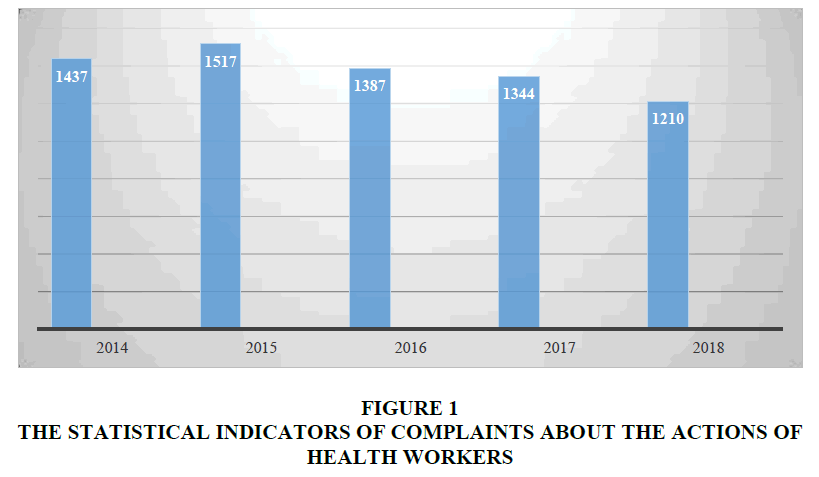
The statistical indicators of complaints about the actions of health workers in the first half of 2019 (271) are almost three times lower than those of the first half of 2014 (701). According to the official figures, the Ministry of Health of Ukraine received 1 210 complaints in 2018, 1 344 in 2017, which is 43 complaints less than in 2016. During the first half of 2019, 271 complaints were registered, compared with 701, which were registered in the first half of 2014 (Figure 1) (Ministry of Health of Ukraine, 2019).
It should be noted that the reduction of complaints is associated with a significant increase in hotline calls and litigation.
For comparison, in 2017 German Service of Medical Insurance (MDK) issued almost 14,000 expert opinions on patients’ complaints about the actions of doctors (Zeit Online, 2018).
In 2013, the Ministry of Health of Belarus received more than 5 800 complaints about the work of doctors. In 2012 there were 4 500 of such complaints. Today, their number has decreased with a corresponding increase of court cases (Spasiuk, 2009).
The number of written complaints lodged in the Public Health Service in the UK between 2015 and 2016 reached 174,900, equivalently to 480 complaints per day. It has been found that certain factors, such as gender and specialty of the doctor, affect the likelihood of receiving a complaint. The indicators show that male physicians receive complaints more often than women, while psychiatrists, general practitioners, and surgeons receive more complaints than other specialties (Wedad & Abdelmageed, 2017).
The number of complaints about medical care in the Russian Federation in 2017 was 6 050, which is 1 100 more than in 2016. In 2012, there were 2,100 of such complaints (Healthcare-In-Europe, 2014).
Some countries have integrated conflict management systems that include mediation. For example, mediator services can be granted by different health care providers. Besides, there is also a difference in the attitude to the institution of mediation and mediation in bioethics between the States. Thus, the United States of America differ in their attitude towards the new method of conflict resolution and the concept of neutrality of an institutionally employed mediator. However, there are three medical mediation organizations in Japan that train more than two thousand people annually. According to Japanese, the training of accredited medical consultants is far more rational than using the services of a bioethics mediator or a mediator (Idrus, 2012).
Any patient can apply to the head of the medical institution, independent public organizations or professional associations, law enforcement agencies or the court with a complaint about the actions of a doctor or the health management body, to resolve the conflict. However, each of these methods has its own characteristics and does not mean that it can satisfy the interests of both parties: the patient and the healthcare provider, quite the contrary-it cannot guarantee the success of the decision (Rozghon, 2016).
Mediation as a way of resolving the dispute arising from patient complaints about the actions of healthcare professionals is a new legal phenomenon for Ukrainian legislation. Today, the mediation procedure in the medical sphere of Ukraine is practically not used. There are several reasons for this:
1. Lack of legislative definition and mediation law;
2. Lack of public awareness;
3. Lack of awareness among patients and doctors of the possibility of using this method of conflict resolution.
Mediation is the processes, in which the parties to the conflict, with the assistance of a neutral mediator, study the problem, identify the ways to resolve it, analyze the options for settlement of the dispute, and choose the most appropriate one for resolving a conflict that would satisfy the interests of both parties (Feoktystov, 2014).
Bioethics mediation involves the resolution of a conflict between a patient or a patient’s relatives and a healthcare professional, and can also be used to resolve disputes between healthcare providers.
Mediation as a way of resolving medical conflicts has many advantages over litigation. They are:
1. The patient and the healthcare provider find and choose the solution that would satisfy the interests of both parties during the mediation process;
2. The outcome of the judgment depends on the professional training of the attorneys, the proper evidence base, and the other personal qualities of the parties;
3. The decision made during mediation is based on the mutual agreement and free will of both parties. The trial is characterized by the opposing features: dispute and evidence.
4. The decision made by the parties (the patient, his representatives, the doctor, and other medical professionals) excludes grounds for appeal, but instead the court decision may be appealed to higher courts.
5. The financial costs for mediation are significantly smaller than the sum of court fees and legal aid costs spent on litigation.
6. The process of resolving conflict through mediation is much faster than litigation.
7. Privacy is an essential principle of mediation. The medical history of the patient becomes known only to the mediator, who is obliged not to disclose information that he (she) became aware of, unlike the lawsuit, the decision of which should be outlined in a single, open to all registry.
8. A decision-making process and its enforcement are free from pressure both on the doctor and on the patient. The execution of the judgments of courts shall be mandatory and can be enforced by coercion.
In its turn, the history of the development of bioethics is the history of the search and creation of a system of universal ethical principles and rules.
Scientists have proposed different systems of principles of bioethics:
1. Autonomous individual, “make good”, justice;
2. “Make good”, the contractual basis for the doctor’s activity, autonomous individual, honesty, the desire to avoid human death and justice;
3. “Make good” and “respect for the autonomous individual”;
4. Justice, faithful to the promises made, truthfulness, charity, “do no harm” (Veatch, 1981).
However, the system of four principles of bioethics is the most widespread and recognized in the theory of this branch of medical science: respect for autonomy, non-maleficence, beneficence, justice, as well as the principles that supply them: veracity, privacy, confidentiality and fidelity. This concept became the starting point and the further discussion of bioethical principles, expansion of their list.
In the past ten years, the ethical discourse has confidently included the principle of integrity, which means:
1. Self-esteem, rejection of corruption, transparency, honesty, friendliness;
2. Intellectual, psycho-spiritual, bodily, genetic integrity of the individual;
3. The inviolability of the individual, the requirement of non-interference in his private sphere (as a legal concept in international legal instruments).
Bioethics is often reduced to a counselor, a medium, a mediator, armed with the modern methods and ways of solving problems, between the representatives of different moral points of view. And in this sense, it is closer to communicative practice (discourse).
The critique of bioethics as a communicative ethic includes the fact that, considering the ethics of life exclusively as a communicative practice, we are forced to some extent to abandon the main value of bioethics-the preservation and development of life. It is necessary to recognize that the main value of communicative practice is still consensus; it is not even a contract or a decision of the majority, but rather, the actualization and positioning of views and values of its participants.
Secondly, does the model of communicative discourse take into account the rights of future generations, the possibility of their participation in the discourse? The future generation cannot give voluntary consent-it has no right to vote. Thus, can the unborn members of society participate in the discourse, have their point of view and defend it.
Besides, it should be noted that the specificity of both mediation and mediation in bioethics is that the patient must give all information about his or her health status and this information will be discussed in the process of conflict resolution. In this case, the question arises of compliance with the moral and ethical standards and the basic principles of bioethics. However, on the other hand, this way of resolving the conflict involves a conversation and hearing both sides to the conflict to reach a consensus peacefully.
Mediation is a consensus, not a compromise. Bioethics mediation means the application of the mediation process to the issues related to clinical conflicts in the health care system. Specificity of mediation in bioethics is the lack of primary interest of the patient. For example, when making decisions about euthanasia, post-mortem donation, the patient is often unconscious and his or her interests are represented by another person (Bachynska, 2014). It should be noted that the ignorance of the will of the patient can negatively affect the fact of the existence of mediation as a whole. However, the formalization and decisions-making in other way, for example, with the involvement of public authorities, can lead to the delay in the process or even to the death of the patient.
The conflicts arising in the medical sphere are characterized by extreme emotionality. Patients and their families are usually persecuted by anxiety and confusion caused by lack of knowledge in medicine, exhaustion, trauma or illness, complexity of medical communication, distrust of the system, negative experiences and feelings of powerlessness (Fiester & Benjamin, 2014). Although mediation cannot completely eliminate the patient’s experience in such cases; it is the existence of a person who hears and responds to the parties’ problems, organizes and explains misunderstandings, and answers questions of the healthcare provider and patients, favorably alters the chances of achieving patient empowerment.
Mediators use appropriate methods and skills to open and improve dialogue between disputes in order to help the parties to reach an agreement on a disputed issue. Generally, all parties should consider the mediator as impartial (Heilbronner, 2018).
Mediator cannot be equated with an arbiter; he (she) ensures proper communication and encourages cooperation. He (she) does not evaluate the situation and make no judgments. To effectively fulfill their role in the process, mediators must have the basics for negotiation. The parties’ perception of the mediator’s neutrality is crucial to success, as the willingness of the parties to disclose information often dependents on the trust that the mediator will not use the information against either party. This is especially true for the patients as they report their health status, medical records and illness. The mediator inspires confidence, in particular, due to his (her) professional status, relevant experience, skills and other personal characteristics.
Speaking about the practice of using mediation in other countries, it should be noted that it was the State of California (the USA) first to talk about mediation as a way of resolving disputes in 1981. An important principle of US mediation is non-disclosure of sensitive information. In view of this fact, the Uniform Mediation Act, which clearly defines, which information could be disclosed and disseminated in the mediation process, was adopted (Uniform Mediation Act, 2003).
In 1979 Nancy Dubler and his colleagues at Montefiore Hospital (New York) began to advocate the use of mediation as the process for resolving disputes among patients, surrogates and family members. The difference of this model of mediation from the traditional one was that it involved a consensus regarding the outcome of the dispute; encouraging all the parties to speak freely; the use of a neutral mediator as a leader in the process of generating options (Bergman & Fiester, 2015).
According to the relevant Italian Legislative Decree, a person who wishes to appeal to court to resolve dispute or to claim compensation for damages caused by health care professionals must first refer to the mediation procedure provided for by the Legislative Decree (Ohrenchuk, 2016).
There were attempts to consolidate mediation in public relations in Ukrainian legislation. For example, the Draft Law of Ukraine “On Mediation” (Draft law of Ukraine, 2019) stipulates that mediation can be applied in any conflicts (disputes), including civil, family, labor, economic, administrative, as well as in criminal proceedings and cases concerning administrative offenses. However, there is no mention of its use in the medical area or in bioethics, which, in our opinion, most in need of the application of this method of conflict resolution. For example, the official website of the Ministry of Health of Ukraine envisages the measures for the proper protection of the rights of the patient, as well as the tips for the further actions in case of dissatisfaction with medical services provided: to contact the police; to go to court; to submit a request for a clinical expert panel, in which the circumstances of treatment should be arbitrarily presented. Thus, the mediation procedure is unavailable of the possible options (Ministry of Health, 2019).
Conclusion
Dynamic indicators of the number of complaints demonstrate the level of patient protection and inviolability of their rights. This requires standardizing the method of analyzing and interpreting patients’ complaints, as well as introducing mediation, which is characterized as a voluntary process whereby a mediator, who has no interest in the dispute, facilitates communication between the patient and the healthcare provider and helps to resolve their conflict peacefully.
One cannot state that in the absence of bioethical mediation the patients’ perspectives will not be heard, and joint decision-making will destroy the traditional model of a doctor as a specialist. The analysis of the legal regulation of the mediation procedure allows indicating the problematic aspects, while the adoption of a special law is only one way to improve the legislation on alternative procedures for conflict resolution. An integrated approach is required to solve the problems and to improve the mediation process, which will involve not only lawyers and academics but also health professionals.
Mediation makes it possible not to bring conflict in public (as in the case of justice), but to solve it private. Besides, it’s time to introduce mediation in bioethics, which has been practiced in other countries for a long time, in Ukraine. Such mediation helps patients or their family members to make difficult choices of appropriate treatment methods.
References
- Bachynska, L.Y. (2014). The Catholic Church’s view on the bioethical problems of abortion and euthanasia: philosophical and legal understanding. International Humanitarian University Herald, 10(1), 34–36.
- Bergman, E.J., & Fiester, A.M. (2015). Mediation. In H. Have (Eds.), Encyclopedia of Global Bioethics. Springer, Cham.
- Chashyna, Z.V. (2015). The analysis of transdisciplinary links in education on the example of bioethics. Integration of Education, 19(1), 100–105.
- Draft Law of Ukraine. (2019). On Mediation of December 17, no. 3665. Retrieved April 27, 2020 from http://search.ligazakon.ua/l_doc2.nsf/link1/JH2TT00V.html
- Feoktystov, ?.V. (2014). Mediation as the way to resolve conflicts. Concept, 27(1), 1–7.
- Fiester, A., & Benjamin, N. (2014). Mediation and the end of clinical ethics as we know it. Cardozo School of Law Journal of Conflict Resolution, 15(2), 501–513.
- Healthcare-In-Europe. (2014). Statistics: Where is there safety in numbers. Retrieved April 27, 2020 from https://healthcare-in-europe.com/en/news/statistics-where-is-there-safety-in-numbers.html
- Heilbronner, R.L. (2018). Mediation. In J.S., Kreutzer, J., DeLuca, B. Caplan (Eds.), Encyclopedia of Clinical Neuropsychology. Springer, Cham.
- Idrus, D. (2012). Private healthcare policy and system in Malaysia and Japan. Retrieved April 27, 2020 from https://www.jil.go.jp/profile/documents/Durrishah_Idrus.pdf
- Ministry of Health of Ukraine. (2019). The analysis of the organization of work with the appeals of citizens, which were submitted to the Ministry of Health of Ukraine in the first half of 2019. Retrieved April 27, 2020 from https://moz.gov.ua/zvernennja-dlja-gromadjan
- Ministry of Health of Ukraine. (2019). The patient has the right: what should be the quality and safe care. Retrieved April 27, 2020 from https://moz.gov.ua/article/health/pacient-mae-pravo-jakoju-mae-buti-jakisna-i-bezpechna-dopomoga
- Ohrenchuk, H.?. (2016). Legal regulation of the use of mediation in the settlement of civil disputes. National Academy of Internal Affairs.
- Potter, V.R. (1971). Bioethics: Bridge to the future. New Jersey: Englewood Cliffs, N. J. Prentice?Hall.
- Rozghon, ?.V. (2016). The ways to resolve conflicts in medical relationship. The Journal of V.N.Karazin Kharkiv National University, 22(2), 123-126.
- Saperov, V.N. (2012). Bioethics or medical ethics? The basic principles of medical ethics. Clinical Medicine, 8(1), 69–72.
- Spasiuk, ?. (2009). Who will protect patients’ rights in Belarus? Belarusian News. Retrieved April 27, 2020 from https://naviny.by/rubrics/society/2009/12/14/ic_articles_116_165850
- Uniform Mediation Act. (2013). National Conference of Commissioners on Uniform State Laws. Retrieved from https://www.uniformlaws.org/HigherLogic/System/DownloadDocumentFile.ashx?DocumentFileKey=9b244b42-269c-769e-9f89-590ce048d0dd&forceDialog=0
- Veatch, R.M. (1981). A theory of medical ethics. New York: Basic books.
- Wedad, A., & Abdelmageed, A. (2017). Understanding patient complaints. Retrieved April 27, 2020 from https://www.bmj.com/content/356/bmj.j452
- Zeit Online. (2018). Number of medical treatment errors is falling. Retrieved April 27, 2020 from https://www.zeit.de/wissen/gesundheit/2018-06/krankenkassen-report-behandlungsfehler-pflegebreich-krankenhaeuser