Research Article: 2021 Vol: 24 Issue: 1S
Medical Interpreter Challenges During In-person Interpretation Session: A Systematic Review
Aisyah Jahidah binti Samsudin, Universiti Sains Islam Malaysia (USIM)
Tg Ainul Farha binti Tg Abdul Rahman, Universiti Sains Islam Malaysia (USIM)
Hayati binti Ismail, Universiti Sains Islam Malaysia (USIM)
Abstract
In a world where geographic boundaries have become blurred lines, & medical treatments can be obtained in all parts of the world, the role of medical interpreters has become increasingly essential roles to attract foreign patients in the medical tourism industry. The medical interpreter acts as a mediator in bridging the gaps between medical teams and patients. However, a medical interpreter's level of ability and skills is often a restriction on an excellent interpretation session to be made. This study aims to analyse medical interpreter challenges during in-person interpretation sessions. A literature review guided by Reporting standards for Systematic Evidence Syntheses (ROSES) is conducted using three databases: Scopus, Dimensions, and Google Scholar. Twenty-five articles are being reviewed after undergoing the identification, screening, and eligibility process of a systematic review. These data have achieved appraisal quality as they have been reviewed by the Critical Appraisal Skill Programme (2018), CASP Qualitative Studies Checklist. Further review of these articles resulted in four main themes: language proficiency skills, communication skills, interaction with medical teams, and interaction with patients. Specific training for overcoming these barriers is suggested to encourage the development of interpreters' role in communication service. This study recommends a quantitative approach in the future to obtain precise results statically.
Keywords
Medical Interpreter, Challenges, In-Person Interpretation, Medical Tourism, Systematic Literature Review
Introduction
Language serves as a conduit for knowledge exchange as it seeks to improve the effectiveness of social interaction. Health tourism has grown to be a significant industry in many countries, greatly contributing to the convergence of national expenditures. This industry, however, cannot avoid involving foreign patients who face contact and language barriers, as it needs cultural and linguistic diversity. The demand for medical interpreters has increased recently as the medical sector continues to grow. The medical interpreter serves as a liaison between international patients and medical teams, bridging the language and cultural divide. As a result, patients will experience increased comfort when seeking treatment in another country.
Generally, many types of interpreting approaches, such as consecutive or simultaneous interpreting, are used to bridge language gaps (Leng et al., 2010). Hornberger, et al., (1996) mentioned that the term "consecutive interpretation" refers to the interpretation given after a speaker has finished speaking, while "simultaneous interpretation" happens when the interpreter simultaneously hears the original speech and interprets it. Additionally, interpretation can be provided in a variety of ways, including in-person, telephonic, video conferencing, and using technological devices. As a result, each method generates a unique set of challenges in effectively transmitting information to patients.
The researcher focuses on in-person interpretation in this study, which occurs face-to-face between the interpreter and the patient. As Michalec, et al., (2015) reported, several patients indicated that having an in-person interpreter would put them at ease, allow for the reception/interpretation of emotions expressed through body language, and increase the intimacy of the conversation. However, a medical interpreter's level of ability and expertise is often a constraint on providing an outstanding interpretation session.
The Significance for a Systematic Review
According to (Shaffril et al., 2019), the systematic review has many advantages over reviews of literature in the traditional style, including the potential to enhance reviews through a simple article retrieving process, a larger and more influential study field, and more critical objectives that can control research bias. This approach increases the chances of coming up with a more precise, focused response to the research question (Mallett et al., 2012).
The present meta-analysis is concentrated upon the following significant research question: What are the in-person medical interpreter challenges during interpretation sessions? The investigation concentrated on the problems encountered by the interpreter. Significantly, this research is needed because there is a lack of analysis of the interpreter's difficulties during in-person interpretation, leading to a restriction for a good interpretation session.
Methodology
This section discusses the four major sub-sections of the current study, including PRISMA, resources, the process of systematic review, and data abstraction and analysis.
Prisma
PRISMA is an acronym of the Preferred Reporting Items for Systematic reviews and Meta-Analyses, a published standard of systematic literature review. This review used this publication standard as it clearly defines the research question. Moreover, it enables the identification of inclusion and exclusion criteria. Plus, it also attempts to examine primary databases of scientific literature within a specific time.
Resources
This review data is derived from three major databases, Scopus, Dimensions and Google Scholar. Generally, Scopus is one of academic literature's largest, most authoritative abstract and citation databases. It contains over 40,000 titles from over 10,000 global publishers, and over 35,000 are peer-reviewed. All Scopus journals are reviewed annually according to four types of numerical quality measurement for each title; h-Index, Cite Score, SJR (SCImago Journal Rank) and SNIP (Source Normalized Impact per Paper). Next, Dimensions is the linked data platform launched in January 2018. Dimensions include multi-source data. Data is converted to a standard data model, cleaned and enriched for use. For many research knowledge databases, data may be skewed towards STEM subjects with more minor arts and humanities information. It is partly due to the relative volume of research activity in these areas and partly due to data availability across different topics—increased coverage in arts, humanities and social sciences. Finally, Google Scholar is a freely accessible online search engine that indexes full text or metadata across many publishing formats and disciplines. The Google Scholar database includes most peer-reviewed scholarly journals and books, conference papers, theses and dissertations, preprints, abstracts, technical studies and other academic literature, including court and patent opinions. An earlier statistical estimate published in PLOS ONE using a mark-and-recapture method estimated around 80–90% of all papers published in English with an estimated 100 million.
The Process of Systematic Review
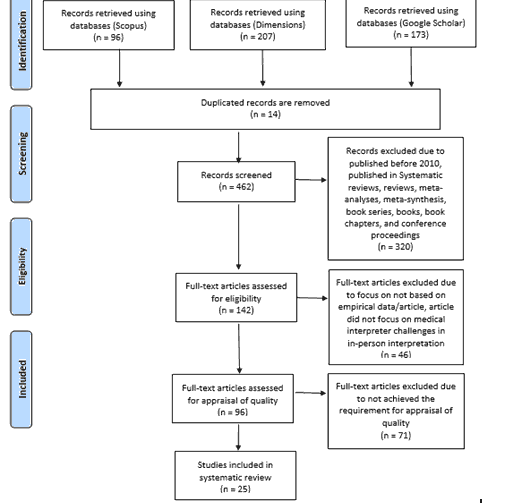
Identification
Three main stages comprise the systematic review method for choosing relevant papers for the current analysis. The first step is to identify keywords, followed by a search for related and similar terms through the thesaurus, dictionaries, and prior research. After defining all related keywords, search strings for Scopus, Dimensions, and Google Scholar databases were established in October 2020 (Refer Table 1). Most notably, the current study could retrieve 476 articles from these three databases successfully.
| Table 1 Search String |
|
|---|---|
| Database | Search String |
| Scopus | TITLE-ABS-KEY(("medical tourism") OR ("health tourism") OR ("medical interpret*") OR ("medical translat*") OR ("health interpret*") OR ("medical translat*") AND ("language* barrier") OR ("communication* barrier")) |
| Dimensions | ("medical tourism" OR "health tourism") ("medical interpreter" OR "medical translator" OR "health interpreter" OR "medical translator") ("language barrier" OR "communication barrier") |
| Google Scholar | "medical tourism" OR "health tourism" OR "wellness tourism" "medical interpreter" OR "medical translator" OR "health interpreter" OR "medical translator." |
Screening
The preliminary screening stage was used to weed out duplicate articles. Fourteen articles were excluded during the first stage, and 462 articles were analysed during the second stage using the researchers' specific inclusion and exclusion criteria. The first specification was the form of literature, and the researchers chose to concentrate solely on journal papers (research articles) since they are the primary sources of empirical evidence. As a result, systematic reviews, reviews, meta-analyses, meta-synthesis, conference proceedings, book series, book chapters, and books were removed from the present study. Plus, the review focused only on English-published articles. It is also important to note that the timeline was established for a 10-year duration (2010-2019). These specifications culminated in excluding 320 articles in total (Refer Table 2).
| Table 2 Inclusion and Exclusion |
||
|---|---|---|
| Criteria | Inclusion | Exclusion |
| Literature type | Article (with empirical data) | Systematic reviews, reviews, meta-analyses, meta-synthesis, conference proceedings, book series, book chapters, and books |
| Language | English | Non-English |
| Timeline | 2010-2019 | <2010 and 2019> |
Eligibility
One hundred forty-two articles were ready for the third stage, dubbed eligibility. On an important note, each article's titles, abstracts, and essential contents were meticulously reviewed to determine they meet the requirements for inclusion and were suitable for use in the current study to meet the research objectives. Consequently, 96 articles are remaining to be reviewed.
Quality Appraisal
The remaining eligibility-related articles must be reviewed to ensure high quality and devoid of bias methodology (Higgins et al., 2019). Mohamed Shaffril et al., 2020 stated that assessing the quality of articles through tools, scales, checklists, or standard forms is a common method. Hence, this study used the Critical Appraisal Skills Programme (CASP) Qualitative Research Checklist. This checklist covers three broad areas: are the results valid, are they worth continuing, and will the results help locally? Ten sub-categories of analysis on the checklist are included to answer these three general questions. These include assessments of the study's objective, methodology, recruiting fit, collection of acceptable and necessary data, the researcher-participant relationship, work ethics, consistency of findings, and research value. Any of the ten sub-categories can be answered with "yes," "can't say," or "no" (see. Figure 1). If the checklist achieved a majority of "yes" answers, the article would be accepted for data synthesis. As a result, 71 articles were excluded, and the remaining 25 articles are ready to be synthesized (see. Figure 2)
Data Extraction and Analysis
The most crucial process is data extraction. Extractions were made following the research question. (Shaffril et al., 2020). Thematic analysis is used to synthesis the data qualitatively. The data compilation was the first step in the theme development process. The authors conducted a thorough analysis of 25 articles to obtain statements or data that answered the research questions. Following that, in the second step, the authors used a coding approach to construct meaningful groups based on the data's nature. In other words, to see suggestive trends or relationships both within and across cases, which can lead to unique analytic paths that guide them to what to look for when they return to their raw data (Sandelowski, 1995). As a result, the process came out with four main themes: namely language proficiency skills, communication skills, interaction with medical teams, and interaction with patients.
Results
General Findings and Background of the Review
The review resulted in six main themes and 24 sub-themes associated with in-person interpretation challenges as presented in Table 3. The four main themes are language proficiency skill (six sub-themes), communication skill (five sub-themes), interaction with medical teams (nine sub-themes), and interaction with patients (five sub-themes). The results provided a comprehensive analysis of the current in-person interpretation challenges.
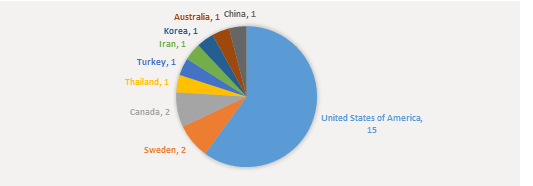
A total of fifteen studies focused on in-person interpretation challenges in the United States of America (Hsieh, 2010; Hsieh & Hong, 2010; Hsieh & Kramer, 2012; Ramsey et al., 2012; Hsieh & Terui, 2015; Ike et al., 2015; Raynor, 2016; Brooks et al., 2016; Kroening et al., 2016; Gutierrez et al., 2017; Krieger et al., 2018; Park et al., 2017; Kamara et al., 2018; Lor et al., 2019; Gutierrez et al., 2019), two studies focused in Sweden (Nkulu Kalengayi et al., 2016; Carlsson et al., 2019 ), two studies focused in Canada (Gabriel et al., 2016; Wu & Rawal, 2017), one study concentrated on in Thailand (Tian & Deocampo, 2017), one study concentrated in Turkey (?ener & Kincal, 2019 ), one study focused in Iran (Fallah & Akbari, 2017), one study concentrated in Korea (Gwag et al., 2017) and one study focused in Australia (Sturman et al., 2018) and one study concentrated on in China (Lin et al., 2016) (see Figure 3).
Main Findings
The discussion in this section centres on four key themes: language proficiency, communication, engagement with medical teams, and interaction with patients, as well as 24 sub-themes that have emerged.
Language Proficiency Skills
This section focuses on the language proficiency skills of a medical interpreter, such as accuracy, dialect, medical terminology, and time constraint.
Accuracy
Accuracy is the most critical issue that is often questioned, as it is an indicator that the information has been delivered precisely. A medical interpreter was expected to interpret without meaningfully adding or subtracting the communication's content and intentions (Tian & Deocampo, 2017). However, the language proficiency skill of medical interpreters is hard to ascertain because there is no certificate or accreditation for medical interpreters since they do not undergo formal training (Krieger et al., 2018). This issue causes the under utilisation of interpretation services (Gabriel et al., 2016) as the physicians' concern about the accuracy of the information been transferred. Carlsson, et al., (2019) found that interpreters had difficulty translating medical words into their native tongue, as there are different linguistic systems between languages (Lor et al., 2019) which made them doubt the services' accuracy.
Dialect
According to García & Sandhu (2015), dialect is generally a subset of a unique language to a particular geographical region or community of people. The pronunciations, grammar, and vocabulary that people use within a community are also referred to as a dialect. Owing to unfamiliar accents or dialects, even from non-native speakers, the medical interpreter often has trouble understanding each other (Sturman et al., 2018). As Lor et al., (2019) reported, medical interpreters have problems interpreting accurately due to various patients' dialects. Subsequently, the patients often request explanations, prompting the interpreter to repeat, rephrase, or clarify. Plus, this situation makes it hard for people to use skilled interpreter services in a wide variety of situations (Ramsey et al., 2012).
Medical Terminology
Medical terminology and medical interpreters are inextricably linked. However, medical interpreters in hospitals have not been trained to interpret medical terminology formally (?ener & Kincal, 2019). Academic credentials, including medical terminology knowledge, do not always qualify interpreters for work in hospitals (?ener & Kincal, 2019). The result obtains by (Lor et al., 2019) suggests that the medical interpreter may need to interject the medical teams and ask for clarification since they might not be familiar with medical terms.
Time Constraint
The difference between written and oral interpreting is the time needed to translate from source language to target language. Since oral interpreting necessitates the ability to translate on the spot, it takes less time to translate than written interpreting. Consequently, it becomes a challenge to the medical interpreter, especially those still a beginner in this field. Moreover, (Tian & Deocampo, 2017) suggested that time constraints compel interpreters to do more than adjust the nuances; they often modify or remove sections of the instructions they are providing. Sturman et al., (2018) also added that the medical interpreter needs more time to offer effectively translated consultations, even though this seems problematic. Hence, this situation leads to inaccuracy of interpretation (Brooks et al., 2016).
Communication Skills
This section focuses on a medical interpreter's language proficiency skills, such as analytical skills, cross-cultural understanding, emphatic linguistic, non-verbal cues, and psycholinguistic.
Analytical Skill
An analytical skill involves analysing information, problem-solving, and decision-making (Hsieh & Terui, 2015). Furthermore, becoming an interpreter means being a competent interpreter in the sense of possessing outstanding language skills and negotiating, logical thinking, and planning skills (Tian & Deocampo, 2017). Interjecting during medical teams-patients consultations when the recipients appear blurred and countering the tone of voice when it was tense (Lor et al., 2019) are examples of how a medical interpreter plays an active role. However, there is a contradictory statement for this issue. Dysart-Gale, 2005, mentioned that the interpreter was supposed to serve as a conduit and a neutral third party, bridging the language gap between medical teams and patients without adding or subtracting information. Plus, medical interpreters often assume that their work as only a voice requires them to be distant, emotionless, and avoid communicating with others (Hsieh & Hong, 2010).
Cross-Cultural Understanding
According to (Nida & Taber, 1969), culture is still intertwined with languages throughout the interpretation process, so a medical interpreter is a culture breaker between medical teams and patients. Hsieh & Terui (2015) suggested that different languages and cultures can have different standards for acceptable speech styles (e.g., direct versus indirect). So, it is essential to understand cultural diversity to avoid offensive communication. Moreover, failure to respect privacy's cultural limits can lead to erroneous conclusions about the speaker's identity or purpose (Hsieh & Terui, 2015). If medical interpreters disagree with the providers' protocol because it is (culturally) inappropriate or ineffective, they will interrupt to translate or change the content of others' narration, which may be troublesome because it could go beyond the providers' medical expertise (Hsieh, 2010).
Clinical Empathy
Clinical empathy is described as the ability to understand patients’ situations, communicate and validate that understanding with them, and then act in a supportive manner (Mercer & Reynolds, 2002). According to (Gutierrez et al., 2019), five empathic linguistic methods are contextualisation, motivation, measuring comprehension, endearment, and softening, and they are used to create interpersonal relationships, promote mutual patient-medical teams understanding and personalised interaction. Still, empathy can go against cultural norms, as some cultures expect direct, not empathic communication with patients, and it becomes challenging for a medical interpreter to maintain a healthy balance between these two roles: human being and professional (Hsieh & Hong, 2010).
Non-Verbal Cue
Nonverbal cues include emotional expressions (Park et al., 2017). They are necessary for effectively conveying information because they often add a touch of feeling and expression to a message, making it seem less stiff. Hence, this statement has opposed the conduit model that needed the medical interpreter to be emotionless and not personally attached to avoid bias. The study that has been demonstrated by (Hsieh & Hong, 2010) found that everyone becomes uncomfortable when a human being acts like a robot because there is nobody's language and no feelings. Furthermore, the facial expression is important because it may indicate whether someone is in distress or not (Kroening et al., 2016).
Interaction with Medical Teams
Another challenge of being a medical interpreter is dealing with the medical teams. This section focuses on the issue that comes from interaction with medical teams such as communication way, inconsistent talk, interpreter mediated communication, lack of respect, negative attitude, not feeling part of the team, not understand interpreter's role, scheduling, and uncooperative manner.
Communication Way
A medical interpreter's role as a third party in channelling information between two parties is not a simple one. Medical interpreters are taught to speak in the first, not the third person (Gwag et al., 2017), so interpreter-mediated communication between medical teams often go wrong. As a result, medical teams can misinterpret what they hear as the interpreter speaking, even though the interpreter is speaking on behalf of the patient (Gwag et al., 2017). Furthermore, it is difficult to concentrate when medical teams speak simultaneously (Park et al., 2017). Plus, when there is contradictory and unclear information (Hsieh & Terui, 2015), when the medical interpreter is relied upon to monitor or restrict the patients' narratives (Hsieh & Kramer, 2012), and when the medical teams cannot tolerate been asked for clarification (Sturman et al., 2018).
Negative Attitude
Not all countries institutionalized a medical interpreter's profession (?ener & Kincal, 2019). It is essential to understand that medical interpreters have always felt like they were not part of the medical team because they are not the core member of the decision-making team, which difficult for them to perform effectively (Wu & Rawal, 2017). Following this, (Park et al., 2017) also added that medical interpreters also felt undervalued and forgotten as medically trained because of their low status within the medical team’s hierarchy. To sum up, it is believed that mutual respect and collaboration between medical teams and interpreters contribute to consultation success. All parties share responsibility for achieving the consultation's objectives, and the patient has the utmost trust in both (Sturman et al., 2018).
Not Understanding the Interpreter’s Role
The medical team did not understand the role of the medical interpreter because of the ambiguity in the role, which can contribute to an unnecessary workload, fueling all participants' frustration in a healthcare interpreting environment and influencing the medical tourism industry's future growth (Gwag et al., 2017). For example, medical interpreters are often asked to complete consent forms on behalf of patients, and medical teams frequently seek them for an opinion on a patient's condition. (Wu & Rawal, 2017), which is out of the conduit role. Hence, a medical interpreter's function is not well known (Krieger et al., 2018), which can stifle the flow of mediated contact between patients and medical teams.
Interaction with Patients
This section focuses on the issue that comes from interaction with patients, such as a problematic understanding interpreter, high demand, keeping up conversation, neutral, trust issue.
Difficulty Understanding the Interprete
Additional difficulties for medical interpreters included terminology that did not have a literal translation in the patient's language or culture and concepts that were not understood or understood differently by patients with low health literacy (Sturman et al., 2018). Thusly, when patients are unfamiliar with the healthcare system, interpreters often provide them with supplementary information or clarification and what medical teams recommend, thus bringing the interpreter out of the shadows (Lor et al., 2019). Consequently, the medical interpreter gets stressed when the patients do not understand (Kalengayi et al., 2016).
Trust Issue
Since it requires the medical interpreter's competence, trust is often an issue between patients and medical interpreters. According to (Ike et al., 2015), patients' mistrust of medical
Interpreters derives from their concerns regarding the accuracy of their interpretations of medical encounters. Besides, (Ramsey et al., 2012) also added that the patients may be hesitant to discuss their medical conditions with strangers. Also, when there is misinterpretation occurs, it might lower the patients’ trust towards the medical interpreters (Kamara et al., 2018) (Table 3 & Figure 3).
| Table 3 Table of Findings |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Language Proficiency Skill | Communication Skill | Interaction With Medical Teams | Interaction With Patients | ||||||||||
| A | D | MT | TC | AS | CCU | CE | NVC | CW | NA | NUIR | DUI | TI | ||
| 1 | Hsieh, 2010 (United States of America) | / | / | / | / | |||||||||
| 2 | Hsieh & Hong, 2010 (United States of America) | / | / | / | / | |||||||||
| 3 | Hsieh & Kramer, 2012 (United States of America) | / | / | / | / | |||||||||
| 4 | Ramsey et al., 2012 (United States of America) | / | / | |||||||||||
| 5 | Hsieh & Terui, 2015 (United States of America) | / | / | / | ||||||||||
| 6 | Ike et al., 2015 (United States of America) | / | ||||||||||||
| 7 | Brooks et al., 2016 (United States of America) | / | / | |||||||||||
| 8 | Gabriel et al., 2016 (Canada) | / | ||||||||||||
| 9 | Kroening et al., 2016 (United States of America) | / | ||||||||||||
| 10 | Lin et al., 2016 (China) | / | ||||||||||||
| 11 | Nkulu Kalengayi et al., 2016(Sweden) | / | / | |||||||||||
| 12 | Raynor, 2016 (United States of America) | / | / | |||||||||||
| 13 | Fallah & Akbari, 2017 (Iran) | / | ||||||||||||
| 14 | Gutierrez et al., 2017 (United States of America) | / | ||||||||||||
| 15 | Gwag et al., 2017 (Korea) | / | / | / | / | / | ||||||||
| 16 | Park et al., 2017 (United States of America) | / | / | / | / | / | ||||||||
| 17 | Tian & Deocampo, 2017 (Thailand) | / | / | / | / | / | ||||||||
| 18 | Wu & Rawal, 2017 (Canada) | / | / | / | ||||||||||
| 19 | Kamara et al., 2018 (United States of America) | / | / | / | / | |||||||||
| 20 | Krieger et al., 2018(United States of America) | / | / | / | / | / | ||||||||
| 21 | Sturman et al., 2018 (Australia) | / | / | / | / | / | ||||||||
| 22 | Carlsson et al., 2019 (Sweden) | / | / | |||||||||||
| 23 | Gutierrez et al., 2019 (United States of America) | / | / | |||||||||||
| 24 | Lor et al., 2019 (United States of America) | / | / | / | / | / | / | |||||||
| 25 | Sener & Kincal, 2019 (Turkey) | / | ||||||||||||
Discussion
The difficulties associated with in-person medical interpretation have been divided into three categories in this section. The first section discusses the difficulties that arise because of the medical interpreter's abilities and skills and how these factors affect the quality of interpretation. Second, it considers the troubles that arise because of the medical team's involvement. The third factor to consider is the difficulties encountered by patients.
The importance of learning a medical language and being fluent in it cannot be overstated, as it is critical for providing safe and efficient treatment for patients (Hull, 2016). Without sufficient initial and continuing training in medical terminology and how to prevent typical interpretation errors, an interpreter can potentially keep making the same number and type of errors for an extended period of time. The exact number and type of errors for an extended period of time (Flores et al., 2012) can affect the accuracy of interpretation. The different dialects made it difficult for foreign patients to comprehend what the medical interpreter said, even though it was correctly translated (Butow et al., 2012). Additionally, time constraints compel the interpreter to alter the utterances' nuances, resulting in a significant disconnect between the role assigned to the interpreter by the hospital staff and actual tasks and linguistic activities performed by the interpreter (Davidson San Francisco, 2000).
Through engaging in and actively communicating with the knowledge present in the patient experience, medical interpreter serves as a mediator and as interpreters-epistemic-brokers work to balance and satisfy the social, communicative, and medical needs on each side of the mediated relationship. (Raymond, 2014). This situation contradicts the commonly held belief that the interpreter's function is limited to bridging the language barrier without imparting conflicting viewpoints or problem-solving to the patient. As the culture breaker, the medical teams were unclear that the interpreter's effort to establish rapport or find culturally appropriate words or analogies to explain scientific concepts to the patients resulted in apparent delays and digressions in some cases (Kaufert & Koolage, 1984). Furthermore, empathy has been described as a cognitive perspective-taking capacity entailing an awareness of another's situation; thus, it is considered beneficial for professional relationships in healthcare experiences because it leads to the encounter's ultimate goal, namely the patient's well-being (Merlini & Gatti, 2015).
Despite explicit guidelines on effective interpreter-mediated clinical communication, most medical teams receive insufficient training on communicating (Hudelson et al., 2012). This condition will lead to confusion when communicating with the patient, such as misinterpretation. Besides, medical interpreters often struggle to challenge providers' viewpoints, which often represent their lower status as a conduit role within the institutional hierarchy (Hsieh et al., 2010), resulting in them being treated as strangers than as a team. Additionally, the interpreter's position is not commonly understood (Krieger et al., 2018), resulting in the medical interpreter being over or underutilized.
"Cultural interpretations" of illnesses are recognised as an obstacle to accessing the most appropriate treatment, as certain foreign patients were reluctant to receive healthcare because they wanted a divine justification rather than a medical explanation of illness (Johnston & Herzig, 2006). As an example, in Malaysia, it can be difficult for the interpreter to clarify to the patient when there are gaps in the health systems of the patient's home country and Malaysia (Kohno et al., 2016). It is a challenging part in merging the gaps in conveying the information. Hence, intercultural training for medical interpreters is necessary to enhance the effective communication with patients. Additionally, patients often cast doubt on interpreters' language proficiency (Edwards et al., 2005), which affects their perceptions about the quality of the information received. Hence, the level of trust in the interpreter was associated with proficiency in medical terminology, education, sharing a shared dialect, showing respect and objectivity, and adhering to the interpreter's code of confidentiality (Hadziabdic et al., 2014).
Recommendations
The results of this systematic review led to numerous suggestions that could benefit future research. First, future researchers should concentrate on other interpretation methods, such as video conferencing and telephone-based interpretation, as this study is constrained to in-person interpretation. Different methods will lead to different perspectives of challenges. Next, future studies may consider using more qualitative designs as they provide in-depth evaluation and detailed medical interpretation challenges. Plus, a quantitative method needs to be done to achieve precise statistical results in analysing a medical interpreter's problems.
Conclusion
Recent research on in-person medical interpretation demonstrates a basic understanding of how challenging the role of a medical interpreter can be, especially when working as a third party in a communication process. Additionally, based on the systematic review, four significant themes representing in-person medical understanding difficulties were identified: language proficiency skill, communication skill, interaction with medical teams, and interaction with patients, each of which was subdivided into 13 subthemes. The first theme concerns the medical interpreter's language proficiency to ensure accurate delivery of information. Second, the theme refers to the medical interpreter's ability to communicate effectively as a mediator between medical teams and patients. The third theme is the interaction with medical teams. The final theme concerns interactions with patients. Therefore, a quantitative method would be increasingly necessary for the future to obtain accurate statistical results.
Acknowledgement
The authors would like to express their gratitude to Ministry of Education (MOE), Malaysia and Universiti Sains Islam Malaysia (USIM) for the support and facilities provided. This research paper project is under grant: (FRGS/1/2019/SSI01/USIM/02/1).
References
- Brooks, K., Stifani, B., Batlle, H.R., Nunez, M.A., Erlich, M., Phil, M., & Diaz, J. (2016). Patient perspectives on the need for and barriers to professional medical interpretation. Rhode Island Medical Journal, 99(1), 30–33.
- Butow, P.N., Lobb, E., Jefford, M., Goldstein, D., Eisenbruch, M., Girgis, A., … & Schofield, P. (2012). A bridge between cultures: Interpreters’ perspectives of consultations with migrant oncology patients. Supportive Care in Cancer, 20(2), 235–244.
- Carlsson, T., Balbas, B., & Mattsson, E. (2019). Written narratives from immigrants following a prenatal diagnosis : qualitative exploratory study. BMC Pregnancy and Childbirth, 19(1), 1–7.
- Francisco, D.S.B. (2000). The interpreter as institutional gatekeeper: The social-linguistic role of interpreters in Spanish-English medical discourse. In Journal of Sociolinguistics 43, 379–405.
- Gale, D. (2005). Communication models, professionalization, and the work of medical interpreters. Health Communication, 17(1), 91–103.
- Edwards, R., Temple, B., & Alexander, C. (2005). Users’ experiences of interpreters: the critical role of trust. Interpreting: International Journal of Research and Practice in Interpreting, 7(1), 77–96.
- Fallah, M., & Akbari, O. (2017). The role of medical translator/interpreter in bringing satisfaction to health tourists at razavi hospital. Razavi International Journal of Medicine, 5(1), 4–6.
- Flores, G., Abreu, M., Barone, C.P., Bachur, R., & Lin, H. (2012). Errors of medical interpretation and their potential clinical consequences: A comparison of professional versus ad hoc versus no interpreters. Annals of Emergency Medicine, 60(5), 545–553.
- Gabriel, P., Ezeaputa, A., Liciu, C., Grant, S., Grant, S., Preston, E., … & Patrick, D. (2016). A pilot study of telephone-based interpretation in family physician offces in British Columbia. BC Medical Journal, 58(8), 433–488.
- García, M.I.M., & Sandhu, A.H. (2015). Language and dialect: Criteria and historical evidence. Grassroots, 49(1), 2003–2017.
- Gutierrez, A.M., Robinson, J.O., Statham, E.E., Scollon, S., & Katie, L. (2017). Portero versus portador : Spanish interpretation of genomic terminology during whole exome sequencing results disclosure. Personalized Medicine, 14(6), 503–514.
- Gutierrez, A.M., Statham, E.E., Robinson, J.O., Slashinski, M.J., Scollon, S., Bergstrom, K.L., … & McGuire, A.L. (2019). Agents of empathy: How medical interpreters bridge sociocultural gaps in genomic sequencing disclosures with Spanish-speaking families. Patient Education and Counseling, 102(5), 895–901.
- Gwag, S., Park, S.Y., Yu, J.H., & Shim, J.L. (2017). Efficient care of oversea patients in clinical practice with a focus on the conflict between healthcare providers and interpreters. International Journal of Applied Engineering Research, 12(23), 13239–13246.
- Hadziabdic, E., Albin, B., & Hjelm, K. (2014). Arabic-speaking migrants’ attitudes, opinions, preferences and past experiences concerning the use of interpreters in healthcare: A postal cross-sectional survey. BMC Research Notes, 7(1).
- Higgins, J.P., Savovi?, J., Page, M.J., Elbers, R.G., & Sterne, J.A. (2019). Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions.
- Hornberger, J.C., Gibson, C.D., Wood, W., Dequeldre, C., Corso, I., Palla, B., & Bloch, D.A. (1996). Eliminating language barriers for non-english-speaking patients. Medical Care, 34(8), 845–856.
- Hsieh, E. (2010). Provider-interpreter collaboration in bilingual health care: Competitions of control over interpreter-mediated interactions. Patient Education and Counseling, 78(2), 154–159.
- Hsieh, E., & Hong, S.J. (2010). Not all are desired: Providers’ views on interpreters’ emotional support for patients. Patient Education and Counseling, 81(2), 192–197.
- Hsieh, E., Ju, H., & Kong, H. (2010). Dimensions of trust: The tensions and challenges in provider-interpreter trust. Qualitative Health Research, 20(2), 170–181.
- Hsieh, E., & Kramer, E.M. (2012). Medical interpreters as tools: Dangers & challenges in the utilitarian approach to interpreters’ roles and functions. Patient Education and Counseling, 89(1), 158–162.
- Hsieh, E., & Terui, S. (2015). Inherent tensions and challenges of oncologist–patient communication: Implications for interpreter Training in Health-care Settings. Journal of Applied Communication Research, 43(2), 141–162.
- Hudelson, P., Perneger, T., Kolly, V., & Perron, N. (2012). Self-assessed competency at working with a medical interpreter is not associated with knowledge of good practice. PLoS ONE, 7(6), 3–8.
- Hull, M. (2016). Medical language proficiency: A discussion of interprofessional language competencies and potential for patient risk. International Journal of Nursing Studies, 54, 158–172.
- Ike, B.R., Calhoun, R., Angulo, A.S., Meischke, H., & Senturia, K.D. (2015). Medical interpreters and bilingual school staff: Potential disaster information conduits? Journal of Emergency Management, 13(4), 339–348.
- Johnston, M.E., & Herzig, R.M. (2006). The interpretation of “culture”: Diverging perspectives on medical provision in rural Montana. Social Science and Medicine, 63(9), 2500–2511.
- Kamara, D., Weil, J., Youngblom, J., Guerra, C., & Joseph, G. (2018). Cancer counselling of low-income limited english proficient latina women using medical interpreters: Implications Z. Journal of Genetic Counseling, 27(1), 155–168.
- Kaufert, J.M., & Koolage, W.W. (1984). Role conflict among “culture brokers”: The experience of native Canadian medical interpreters. Social Science and Medicine, 18(3), 283–286.
- Kohno, A., Farid, N.D.N., Musa, G., Aziz, N.A., Nakayama, T., & Dahlui, M. (2016). Factors affecting Japanese retirees’ healthcare service utilisation in Malaysia: A qualitative study. BMJ Open, 6(3), 1–8.
- Krieger, M., Agather, A., Douglass, K., Reiser, C.A., & Petty, E.M. (2018). Working with the Hmong population in a genetics setting: An interpreter perspective. Journal of Genetic Counseling, 27(3), 565–573.
- Kroening, A.L.H., Moore, J.A., Welch, T.R., Halterman, J.S., & Hyman, S.L. (2016). Developmental screening of refugees : A qualitative study. Pediatrics, 138(3).
- Leng, J.C.F., Changrani, J., Tseng, C.H., & Gany, F. (2010). Detection of depression with different interpreting methods among Chinese and Latino primary care patients: A randomized controlled trial. Journal of Immigrant and Minority Health, 12(2), 234–241.
- Lin, L., Brown, K.B., Hall, B.J., Yu, F., Yang, J., Wang, J., … & Wong, F.Y. (2016). Overcoming barriers to health-care access: A qualitative study among African migrants in Guangzhou, China. Global Public Health, 11(9), 1135–1147.
- Lor, M., Bowers, B.J., & Jacobs, E.A. (2019). Navigating challenges of medical interpreting standards and expectations of patients and health care professionals : The interpreter perspective. Qualitative Health Research, 29(6), 820–832.
- Mallett, R., Zanker, H.J., Slater, R., & Duvendack, M. (2012). The benefits and challenges of using systematic reviews in international development research. Journal of Development Effectiveness, 4(3), 445–455.
- Mercer, S.W., & Reynolds, W.J. (2002). Empathy & quality of care. British Journal of General Practice, 52(SUPPL.), 9–12.
- Merlini, R., & Gatti, M. (2015). Empathy in healthcare interpreting: Going beyond the notion of role. Interpreters Newsletter, 20, 139–160.
- Michalec, B., Maiden, K.M., Ortiz, J., Bell, A.V., & Ehrenthal, D.B. (2015). Providers’ Perceptions of medical interpreter services and Limited English Proficiency (LEP) Patients: Understanding the “Bigger Picture.” Journal of Applied Social Science, 9(2), 156–169.
- Shaffril, H.A., Samah, A.A., Samsuddin, S.F., & Ali, Z. (2019). Mirror-mirror on the wall, what climate change adaptation strategies are practiced by the Asian’s fishermen of all? Journal of Cleaner Production, 232, 104–117.
- Shaffril, H.A., Samsuddin, S.F., & Abu Samah, A. (2020). The ABC of systematic literature review: The basic methodological guidance for beginners. Quality and Quantity.
- Nida, E., & Taber, C.R. (1969). The theory and practice of translation. In Leiden: EJ. Brill.
- Kalengayi, N.F.K., Hurtig, A., Nordstrand, A., Ahlm, C., & Ahlberg, B.M. (2016). Perspectives and experiences of new migrants on health screening in Sweden. BMC Health Services Research, 16(1), 1–13.
- Park, E.R., Mutchler, J.E., Perez, G., Goldman, R.E., Niles, H., Haime, V., … & Pirl, W.F. (2017). Coping and Resiliency Enhancement Program (CARE): A pilot study for interpreters in cancer care. Psycho-Oncology, 26(8), 1181–1190.
- Ramsey, K.W., Davis, J., & French, G. (2012). Perspectives of chuukese patients and their health care providers on the use of different sources of interpreters. Hawai’i Journal of Medicine & Public Health, 71(9), 249–252.
- Raymond, C.W. (2014). Epistemic brokering in the interpreter-mediated medical visit: Negotiating “Patient’s Side” & “Doctor’s Side” Knowledge. Research on Language and Social Interaction, 47(4), 426–446.
- Raynor, E.M. (2016). Factors affecting care in non-english- speaking patients and families. Clinical Pediatrics, 55(2), 145–149.
- Sandelowski, M. (1995). Qualitative analysis: What it is and how to begin. Research in Nursing & Health, 18(4), 371–375.
- ?ener, O., & Kincal, ?. (2019). Role and ethics in healthcare interpreting in Turkey. Journal of Translation Studies and Applications,27, 201–219.
- Sturman, N., Farley, R., Claudio, F., & Avila, P. (2018). Improving the effectiveness of interpreted consultations : Australian interpreter, general practitioner & patient perspectives. Health and Social Care in the Community, 26(2), e233–e240.
- Tian, X., & Deocampo, M.F. (2017). A linguistic analysis of chinese patients’ attitudes using appraisal theory as reflected through translation. The New English Teacher, 11(2), 40.
- Wu, M.S., & Rawal, S. (2017). “Its the difference between life and death ”: The views of professional medical interpreters on their role in the delivery of safe care to patients with limited English proficiency. PLoS ONE, 12(10), 1–11.
- Nida, E., & Taber, C.R. (1969). The theory and practice of translation. In Leiden: EJ. Brill.Higgins, J.P., Savovi?, J., Page, M.J., Elbers, R.G., & Sterne, J.A. (2019). Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions.