Research Article: 2021 Vol: 24 Issue: 6S
Professional Responsibility in Thyroid Surgery: Complication or Error?
Maricla Marrone, Università degli Studi di Bari Aldo Moro
Alessandra Stellacci, Università degli Studi di Bari Aldo Moro
Gaetano Achille, Università degli Studi di Bari Aldo Moro
Ettore Gorini, Università degli Studi di Bari Aldo Moro
Luigi Buongiorno, Università degli Studi di Bari Aldo Moro
Benedetta Pia De Luca, Università degli Studi di Bari Aldo Moro
Ferorelli Davide, Università degli Studi di Bari Aldo Moro
Gerardo Cazzato, Università degli Studi di Bari Aldo Moro
Laura Marrone, Università degli Studi di Bari Aldo Moro
Pierluigi Caricato, Università degli Studi di Bari Aldo Moro
Leonardelli Mirko, Università degli Studi di Bari Aldo Moro
Stefania Lonero Baldassarra, Università degli Studi di Bari Aldo Moro
Francesca Tarantino, Università degli Studi di Bari Aldo Moro
Angela Pezzolla, Università degli Studi di Bari Aldo Moro
Francesco Vinci, Università degli Studi di Bari Aldo Moro
Alessandro Dell’Erba, Università degli Studi di Bari Aldo Moro
Abstract
Thyroidectomy is an operation with a high percentage of post-operative complications that can lead to severe disabilities. This leads to a high number of claims which often do not translate into objective assessments by Consultants and Judges. In light of these data and the frequent litigation in the surgical field, the authors examined ten sentences issued between 2018 and 2021 relating to claims for damages for alleged health malpractice. This article aims to examine the nature of the compensation claims for alleged health malpractice in the field of thyroid surgery and to offer ideas for an objective assessment based on the legislation in force in Italy.
Keywords
Thyroid Disorders, Thyroidectomy, Health Malpractice, Damage Assessment
Introduction
Thyroid disorders result from alterations or dysfunctions of the thyroid gland, an endocrine gland that produces the thyroid hormones, thyroxine (T4) and triiodiothyronine (T3).
Triiodiothyronine is the active form of the hormone and makes up 20% of the total thyroid product. The remaining 80% is T4, which is kept in this form, ready to be converted into T3 according to the needs of the body.
According to recent data, one in 3,000 newborns has a thyroid disease.
In adulthood, women are much more likely to develop thyroid disease than men: A woman has about a 20% chance of developing thyroid disease in her lifetime (Campo, 2013; Higher Institute of Health, 2019).
The increase in thyroid volume is defined as goiter (Higher Institute of Health, 2020).
This can be uninodular or multinodular or it can result from a diffuse increase in the glandular parenchyma.
Thyroid nodules are usually benign (only 7% is malignant neoplasm).
The most common carcinomas are papillary or papillary-follicular (mixed) and follicular carcinomas which alone account for about 65-70% of malignant thyroid tumors.
Over 90% of them recover.
Thyroid cancers are more common among women than men, with an M: F ratio of 1: 3.2 and its incidence increases with age2.
The surgeon's experience, knowledge of thyroid anatomy and thyroid pathology are important elements in the field of thyroid surgery.
In fact, while mortality secondary to thyroid surgery is rare, complications can lead to serious outcomes (Gopalakrishna & Shaha, 2010; Al-Fakhri et al., 1998; Rosato et al., 2000).
Hypoparathyroidism is the most frequent complication of thyroid disease with percentages in literature between 0% and 10% (on average 2%).
Both unilateral and bilateral recurrent nerve injuries are reported with a frequency of 0 to 8%. Dysphagia, usually transient, can cause ab ingestis bronchopneumonia.
Hemorrhage has an incidence of 0.1%-3.8%, while that of infections is about 1% (Efremidou et al., 2009).
In light of these data and the frequent litigation in the surgical field, the authors examined ten sentences issued between 2018 and 2021 relating to claims for damages for alleged health malpractice.
Aim and Scope
This article aims to assess the nature of the compensation claims for alleged health malpractice in the field of thyroid surgery in Italy.
In particular, in light of the new Italian regulations on the subject (Law 24/2017), we asked ourselves what they were:
• the characteristics of the disputes established;
• the alleged damages most often reported;
• any reprehensible conduct of health professionals;
• the reasons for accepting or rejecting the request for compensation.
Materials and Methods
A retrospective study was conducted using the Pluris Wolters Kluwer legal database as well as the Telematic Services Portal (PST) to search for judgments.
We have randomly selected ten sentences issued from 2018 to 2021 in Italy regarding claims for compensation following thyroid surgery.
The terms "thyroid", "thyroidectomy" and "health responsibility" were used to select the sentences then analyzed.
The content of the sentences was then examined in detail also for the aspects concerning the outcome of the Judge's decision.
The Pluris Wolters Kluwer database is an online legal research, information and updating system for lawyers.
It is a professional tool that allows access to regulations and judgments, but also to comments on articles and laws.
It is a constantly updated search system which, upon subscription, allows searches for judgments and maxims; authoral comments on the articles of the main codes; scientific articles, procedural assistance and full texts relevant to research.
The Portal of Telematic Services (PST) of the Ministry of Justice, on the other hand, is a tool that allows the search and display of judgments of merit only to those registered in the REGINDE, without the need for a subscription.
The following characteristics of greatest importance in the research in question were therefore examined:
Competent court and date of delivery of the sentence;
• the sex and age of the plaintiff/applicant
• the underlying pathology
• the type of intervention undergone
• the alleged damage reported,
• the outcome of the dispute
• the damage recognized (in case of acceptance of the request for compensation)
• the motivation of the sentence.
These data are shown in table 1.
However, even for the Italian privacy legislation which is severe (in favor of the protection of the rights of individuals), some data relating to the plaintiff/plaintiff were not found.
In all the judgments the outcome and motivation of the same was clarified.
This aspect is fundamental as it allows tracing some recurring characteristics.
| Table 1 Characteristics Analyzed |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Court | Date of judgment | Gender/age of appellant | Disease | Type of surgery | Alleged damage | Outcome of the Judgment | Compensation awarded | Grounds of the judgment | |
| 1 | Court of Palermo | Apr. 2018 | M - 50 | Goiter | Total thyroidectomy | Vocal cord paralysis | Negative | None | Complication |
| 2 | Court of Latina | Nov. 2018 | F - n.d. | N.d. | Total thyroidectomy | Dysphonia, dysphagia. | Negative | None | Complication |
| 3 | Court of Potenza | Nov. 2019 | F - n.d. | Cyst and thyroid enlargement | Total thyroidectomy | Dysphonia, dysphagia | Negative | None | Very complicated surgeries |
| 4 | Court of Palermo | July. 2020 | F - 64 | Goiter | Total thyroidectomy | Dysphonia, dysphagia and hypocalcaemia | Positive | 20%(biological damage) 59.800,00 €+Customization 5%+3.920 € temporary disability (total for 10 days, partial disability at 50% of 60 days)+514,51 € health expenditure | Failure to prepare laryngeal nerve |
| 5 | Court of Roma | Dec. 2020 | F - n.d. | Goiter/carcinoma | Total thyroidectomy | hypocalcaemia | Negative | None | Complication |
| 6 | Court of Novara | Mar. 2021 | F - 67 | Goiter | Total thyroidectomy | Dysphonia, dysphagia | Negative | None | Complication |
| 7 | Court of Roma | Mar. 2021 | F - 47 | N.d. | Total thyroidectomy | Dysphonia dysphagia and aesthetic damage | Positive for dysphonia dysphagia, negative for aesthetic damage | 10% (biological damage) total temporary disability for 40 days and partial disability 50% for 45 days 24.171,28€ | Bad identification/ overstretching of the laryngeal nerves |
| 8 | Court of Rovigo | Apr. 2021 | F - n.d. | N.d. | Total thyroidectomy | Vocal cord paralysis | Positive | 30% (biological damage) 134.915,00 €+ 3.712,50 € per for temporary disability (75% for 30 days, 50% for 30 days) | Bad identification of the laryngeal nerves |
| 9 | Court of Napoli | May-21 | F - n.d. | Goiter | Total thyroidectomy | Vocal cord paralysise and dispnea | Negative | None | Complication |
Statistic Analysis
Statistical analysis was conducted using Microsoft Excel 2013 software (Microsoft Corporation, Redmond, WA, USA) and IBM SPSS Statistics version 25 for windows (IBM Corporation, Armonk, NY, USA).
The categories examined were then represented in percentage terms.
Conclusion
Nine judgments issued from 2018 to 2021 and related to thyroid surgery were examined.
All concerned total thyroidectomy operations undergone by female individuals in 8 cases (88.9%) and in one case by a male individual (11.1%).
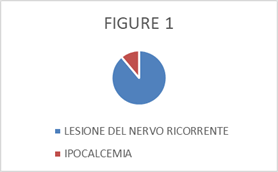
In eight cases (88.9%) the complaint was due to recurrent nerve injury, in another case (11.1%) to hypocalcemia (Figure. 1).
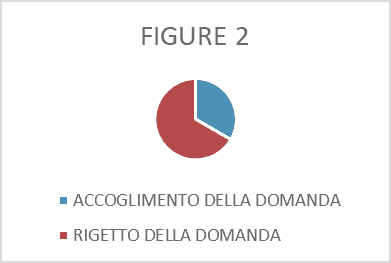
Of the nine rulings, three resulted in an acceptance of the plaintiff/plaintiff's request (33.3%) and six rejected it (66.7%) (Figure. 2).
The decisions that accepted the request for compensation were all motivated on the basis of the gaps in the medical record, in particular with regard to the description of the surgery performed: the absence of a detailed description of how the identification and preparation were carried out of the laryngeal nerves, in the technique performed, was a source of attribution of responsibility.
In other words, in the face of nerve damage, the failure to describe operational accuracy has favored the hypothesis of absence of the same by the operator.
The data that emerges, therefore, is that most of the claims for compensation were considered well founded if no elements emerged from the medical record (and the description of the intervention contained therein) that made it possible to assess the correctness of the conduct of health professionals.
In Italy, "the medical record drawn up by the doctor of a public health facility has the nature of a public act with privileged faith ... with reference to the facts attested by it" (Court of Cassation, Criminal Section V, Sentence 11 September 2013 n. 37314).
At the same time, "the incompleteness of the medical record is a factual circumstance that the judge can use to consider the existence of a valid causal link between the doctor's work and the damage suffered by the patient only when such incompleteness has made impossible the 'ascertainment of the related etiological link and the professional has in any case put in place a conduct that is abstractly suitable to cause the damage "(Court of Cassation Section III Civil, Sentence November 14, 2019 n. 29498) therefore, should it not be possible to reconstruct the incompleteness of the file the intervention and the cause of the injury remained unknown, there would be a sort of inversion of the burden of proof, dictated by the principle of proximity of the evidence, such that the lack of proof of the origin of the harmful event would fall on the health facility. (see Court of Cassation, Civil Section III, 12 June 2015 n. 12218 and 21 November 2017 n. 27561)
In our procedural system, only once the injured party has demonstrated that the worsening of the pathological situation, the onset of new pathologies or even the death is causally attributable to the work of the health workers, arises, for the health facility and/or for the doctor, the burden of proving that the non-fulfillment does not exist or has been caused by a non-attributable cause.
In the cases examined, which ended favorably for the injured party, the doctors were unable to demonstrate the correct fulfillment of the service performed and that the non-fulfillment was due to causes not attributable to them.
Instead, it was demonstrated by the injured party that the conduct of the health workers was suitable for determining the damaging event, in line with what was established by the previous judgments of legitimacy (Court of Cassation, Section III Civil, sentence 5 - 26 July 2017, n. 18392 ; Court of Cassation, Civil Section III, judgment no. 26824 of 14 November 2017; Court of Cassation, Civil Section III of 7 December 2017, no. 29315; Court of Cassation, Civil Section III, February 15, 2018, no. 3704 ; Court of Cassation, Civil Section III, 23 October 2018, no. 26700, Court of Cassation, Civil Section III, 11 November 2019, no. 28991).
On the contrary, in the remaining cases examined, the completeness of the medical record led the Judge's auxiliaries to evaluate the behavior of the health professionals/surgeons as correct.
Infact, the alleged damage was considered in these cases as a non-attributable complication.
The Court of Cassation focused on the concept of complication in Italy, stating that “With the term “complication”, clinical medicine and forensic medicine usually designate a harmful event… which, although abstractly foreseeable, would not be avoidable. This concept is useless in the legal field. When, in fact, during the execution of an intervention or after its conclusion, a worsening of the patient's condition occurs, either: - or this worsening was foreseeable and avoidable, and in this case it must be ascribed to fault of the doctor, not at all, noting that the clinical statistics theoretically include it among the "complications", or this worsening was not foreseeable or was not avoidable: and in this case it integrates the details of the "non-attributable cause" referred to in 'article 1218 of the civil code, not at all, noting that clinical statistics do not theoretically include it among the "complications". The law does not care whether the harmful event unwanted by the doctor falls within the clinical classification of complications or not: it only matters whether that event integrates the details of the "non-attributable cause" ... The circumstance that an undesired event is qualified by the clinic as a "complication" it is not enough to make it in itself a "non-attributable cause" pursuant to article 1218 of the civil code; just as, on the other hand, events that do not qualify as complications can theoretically constitute fortuitous cases that exclude the doctor's fault. From the foregoing it follows, on the level of evidence, that in the judgment of responsibility between patient and doctor: - either the doctor manages to demonstrate that he has behaved in compliance with the leges artis, and then he is exempt from liability at all, noting that the damage suffered by the patient does or does not fall into the category of "complications"; - or, on the contrary, the doctor fails to provide that evidence: and then he will not benefit from the fact that the damage event is in the abstract unpredictable and inevitable, since what is relevant is whether it was foreseeable and avoidable in the specific case. Predictability and avoidability of the concrete case which, for what has been said, it is the doctor's responsibility to prove ". (Court of Cassation, Civil Section III, 30 June 2015, No. 13328).
In one of the cases examined, the responsibility was not attributed to the doctors due to the particular difficulty of the specific case (sentence 3 of table 1).
Infact, the thyroid was of such size as to alter the anatomical relationships of the gland.
Then the cause of the alleged damage (dysphonia and dysphagia) was attributed to the lesion of the recurrent nerve, which was not identified during the operation, but the request for compensation was not accepted, since the doctors, in the conditions in which they found themselves operating, they could not avoid what actually happened.
In fact, in Italy pursuant to art. 2236 of the Italian Civil Code "If the service involves the solution of technical problems of special difficulty, the contractor is not liable for damages, except in the case of willful misconduct or gross negligence".
In our country, in the area of health responsibility, this rule does not apply in the event of damage attributable to the negligence and imprudence of the professional, but is limited to cases of inexperience attributable to the particular difficulty of technical problems that the professional activity, in practice, makes it necessary to face (Court of Cassation, Civil Section III, April 19, 2006, n. 9085), with the clarification that, based on the principle of proximity to the evidence, it is up to the doctor to prove the particular difficulty that characterized the case (Court of Cassation, Civil Section III, 9 November 2006, n. 23918).
Let us briefly recall infact that the recurrent nerve (or inferior laryngeal nerve) is made up of somatomotor, somatosensory and visceral fibers.
It has a sphincter (protection of the respiratory tract from foreign bodies), respiratory and speech functions (Crinò & Gualniera, 1994).
The complexity of the anatomical relationships that the nerve contracts in its course can present a problem for the surgeon.
However, it has long been known that careful isolation of the nerve extremely reduces the risk of injury (Hayward et al., 2012; Lahey, 1983; Riddel, 1970).
Recurrent nerve injuries typically result from ischemic or mechanical insults (Mattotti, 1985).
In the case examined, the pathological changes in the thyroid made the recognition and isolation of the recurrent nerve particularly difficult and for this reason the doctors were relieved of responsibility.
In general, however, the boundary between avoidable error and complication is blurred, too often entrusted to the subjective interpretation of the Judge in turn induced by the equally subjective evaluation of his auxiliary technical consultant.
If from 2017, following the entry into force of specific legislation (Law 24/2017), disputes relating to health responsibility, in Italy, are technically judged by a panel always consisting of a Legal Doctor to whom supporting the branch specialist, with “proven experience”, and so much favored a more detailed analysis of the proposed story, everything that was previously judged often lacked this double evaluation, which is indispensable, in the opinion of the authors.
Clinical experience in the field of thyroid surgery can make it possible to evaluate, based on what is reported in the medical record and what is objectivable in the opinion of the expert, if you are faced with a mere unavoidable complication, despite the surgeon's precautions, or whether an avoidable error has occurred on the part of the surgeon.
The associated medical-legal expertise will make it possible to better define the boundaries of these terms (complication/error) avoiding clinical confusions, not transportable in a legal context.
In addition, the Legal Doctor will be able to quantify the alleged and objected damage to an appropriate extent
Nonetheless, however, in the face of a standard thyroid surgery (not burdened by particular technical difficulties) producing, however, damage to the recurrent nerve, which and how many elements must be considered?
With what degree of importance?
Was proper nerve identification done?
Was the same isolated just as correctly?
So much is it documented in the folder?
How long after functional symptoms did they start?
Was a post-operative specialist evaluation performed?
What type of nerve damage was it?
Partial injury, strain or complete injury?
Was it bilateral or unilateral?
Did the site of damage correspond to the site of intervention?
Were there pathological pre-existences incident on the current complained picture or on the success of the surgery performed?
And if it is not possible to answer all these questions and any further evaluable for the specific case, can the opinion expressed be considered objective or vitiated by an evaluative subjectivity that is not suitable in court?
Too often, infact, claims for compensation following surgery for thyroid pathologies have different evaluation outcomes based on the Judge (meaning both the Judge himself and his technical assistant) so much it favors an evident difference in attitude towards the health workers operating, with consequent also difficult management of medical work.
If the clinical distinction between predictable but not preventable complication (therefore not attributable to the healthcare professional) and error is often not easy, certainly easier, as well as more "objective" is this distinction made on the basis of above all legal criteria such as, for example, those related the completeness of the medical record, with particular reference to the documentary description provided by the operating report.
Can a correct keeping of the medical record therefore “save” a healthcare professional from the judgment of professional responsibility even in the face of damage to the patient?
Very often yes, hoping that those who read and interpret in turn what is reported in that folder, have the appropriate skills to judge it.
And always those who "read", or those called to evaluate the work of the health workers, must also have the appropriate skills in relation to the percentage assessment of the damage.
Infact, a further important element emerging from the proposed analysis is the important valuation discrepancy: the percentages of damage recognized in the judgment show a very wide range that fluctuates between 30 and 8%.
Unfortunately, the reading, albeit in-depth, of the sentences does not allow us to trace exactly how this percentage was assessed (by the technical auxiliary) and therefore it is not possible to provide detailed considerations on the matter, but it is common experience that this evaluation area is also affected by criteria too often subjective.
It is hoped that in the future the importance of using a panel of "experts" (both in clinical and medical-legal matters) as technical auxiliaries to the Judge in cases of professional liability will be increasingly affirmed and that therefore the criterion choice is not based only on the certificate of "specialist" title, but the experience in the specific sector is evaluated.
So much so in order not only to produce sentences as close as possible to objective criteria, but also to favor a more serene medical operative activity.
A further hope, however, is to seek technical-scientific guidelines which, while respecting the aforementioned regulations and provisions of the Supreme Court, can allow the judge's auxiliaries to express themselves technically (and not only juridically) on the correctness of the health behaviors examined, having precise references in this regard.
Conflict of Interest
There isn’t any conflict of interest.
References
- Campo S., Cricelli C., Lapi F., Medea G., & Pecchioli S. (2013). Thyroid pathology in Italian General Medicine. Epidemiological study and considerations on the patient's clinical management. Review of Ethical Issues in Medical Genetics, 2, 7–11.
- Higher Institute of Health. (2019). Epidemiology for public health. Thyroid diseases.
- Higher Institute of Health. (2020). Epidemiological data. Goiter
- Higher Institute of Health. (2020). Epidemiology for public health. Goiter
- Gopalakrishna, I.N., & Shaha, A.R. (2010). Complications of thyroid surgery: Prevention and management. Minerva Chirurgica, 65(1), 71-82.
- Al-Fakhri, N., Schwartz, A., Runkel, N., & Buhr, H.J. (1998). Rate of complications with systematic exposure of the recurrent laryngeal nerve and parathyroid glands in operations for benign thyroid gland diseases. Central sheet for surgeons, 123(1), 21-4.
- Rosato, L., Mondini, G., Ginardi, A., Clerico, G., Pozzo, M., & Raviola, P. (2000). Incidence of complications of thyroid surgery. Minerva Chirurgica, 55(10), 693-702.
- Efremidou, E.I., Papageorgiou, M.S., Liratzopoulos, N., & Manolas, K.J. (2009). The efficacy and safety of total thyroidectomy in the management of benign thyroid disease: A review of 932 cases. Canadian Journal of Surgery, 52(1), 39-44.
- Crinò, C., & Gualniera, P. (1994).The recurrent damage in thyroid surgery. Medico-legal aspects. Revista da Legal Medicine.
- Hayward, N.J., Grodski ,S., Yeung, M., Johnson, W.R., & Serpell J. (2012). Recurrent laryngeal nerve injury in thyroid surgery: A review. ANZ Journal of Surgery, 83(1-2),15-21.
- Lahey, F.H. (1983). Routine dissection and demonstration of recurrent laryngeal nerve in sub-total thyroidectomy. Surgery, Gynecology & Obstetrics, 66(775).
- Riddel, V. (1970). Thyroidectomy – Prevention of bilateral recurrent nerve palsy. British Journal of Surgery, 1, 57.
- Mattotti, M. (1985). Mechanisms of recurrent damage, IX Conv. Aggiornamento A.O.O.I. Udine. Italy.