Research Article: 2021 Vol: 20 Issue: 5
The Management of Behavior Considerations for Acceptance and Uptake of Covid-19 Vaccines among Nurses in Thailand
Buppachat Urairak, Shinawatra University
Abstract
The objective of this research was to study factors affecting the behavior for acceptance and uptake of COVID-19 vaccines among nurses in Thailand. The sample group used in this research consists of 400 professional nurses residing in Thailand. The data was collected using questionnaires with a reliability coefficient of 0.837. The statistics used in this research were the descriptive statistics. The hypotheses were tested using t-test, Pearson Correlation, and Multiple regressions. The research results revealed that regarding the eligibility of COVID-19 vaccine type did not influence the decision to get vaccinated at the statistical significance level of 0.05. The independent variables influenced the decision of acceptance and uptake of vaccine of nurses in Thailand a little with the influence value of only 8.7%, while the social influence factors and environmental factors were influencing factors with the influence value of 0.248 and 0.191, respectively. As the sample group was registered nurses with medical knowledge, they had greater confidence in their own decisions rather than influences from other factors. It was found that the level of behavior of acceptance and uptake of COVID-19 vaccine among Thai nurses was high at the significant level of 0.05 with the mean of 4.18. Therefore, Thailand should formulate the strategies in urgently finding the vaccines and accelerating the COVID-19 vaccination rate among healthcare professionals and registered nurses as quickly as possible in order to help building the confidence among the general public. This will lead to herd immunity in Thailand in an efficient and effective manner and in timely fashion to solve the current critical situation.
Keywords
COVID-19, Vaccines, Acceptance, Uptake, Nurses.
Introduction
With the covid-19 pandemic, more than 1 million people have died within less than nine months after the first outbreak was reported in Wuhan, china. The number of infections continues to rise at an unprecedented rate due to the speed of dangerous transmission. The covid-19 epidemic is the deadliest pandemic in 100 years after the Spanish flu. Same as previous disease outbreaks, scientific research is an important key in fighting against covid-19 through drug development and other treatments. There has to be an effort to create an effective vaccine to tackle this novel coronavirus as a mean to bring the world back from the recession and a better quality of life. The global vaccine development efforts in response to the covid-19 pandemic is unprecedented in terms of scale and speed of the development to provide an indication that the vaccine can be quickly used in emergency cases within the year 2021. It changes the steps from conventional vaccine development to innovative vaccine development (Bunyavejchewin & Sirichuanjun, 2021; Kaur & Gupta 2020; Le et al., 2020).
According to the meeting results of who technical advisory group(tag) on October 15, 2020 on the behavioral considerations in relation to covid-19 vaccine acceptance and uptake, it was found that focusing on changing the behaviors of vaccine acceptance in the population group of the country in order to achieve the goal depends on the behaviors of the group of leaders in the healthcare service providers who offer vaccine administration policies, plan on the vaccination and the strategies to create the most vaccine uptakes. It depended on the group of influencing people indecision-making to create the confidence of vaccine uptake. Who is not responsible for the content or accuracy of this translation). Who’s behavioral research found that 3 factors affect the vaccine uptake apart from the knowledge everyone is required to have; 1. An enabling environment 2. Social influences and 3. Motivation promoting each factor using them in combination will further contribute to the success of the acceptance and uptake of the covid-19 vaccine (WHO, 2020). The covid-19 pandemic, the ever-changing prognosis, the severe lack of resources to treat and protect healthcare providers from infection, standardize unfamiliar public health standards and the restriction of individual freedom are the important factors that put pressure on emotional distress and the risk of psychiatric illness. The healthcare providers play an important role in managing these emotions. The healthcare providers have to communicate risk prevention guidelines and educate about vaccine efficacy as well as be the leaders in generating reliable vaccine acceptance (Pfefferbaum & North 2020). In Thailand, there were survey results on the opinions of healthcare professionals and public health personnel on covid-19 vaccine of the Health Intervention and Technology Assessment Program (HITAP), health system research institute, ministry of public health. The survey was conducted from 29 Jan. To 16 Feb. 2021 with 55,068 questionnaire respondents. The survey results revealed that 55% were willing to receive the vaccine. The first preferred vaccine was AstraZeneca while the 2nd place was Sinovac. The 3rd place was Pfizer-Biotech and the 4th places were Moderna and Johnson & Johnson. The 5th place was Gamaleya. It was also found that the key conclusion was that 55% of healthcare providers and public health providers were willing to receive any vaccine. 35% were uncertain about taking vaccine or not while 10% did not want the vaccination. The healthcare providers, nurses, pharmacists, dentists and physicians were the highest percentage likely not to receive the vaccine or unsure. Only 47% of nurses were willing to receive the vaccine. Knowing that there were people previously vaccinated without serious side effects is a key condition that increases the vaccine acceptance rate by 90% (HITAP, 2021). The cumulative number of received vaccinations in Thailand (Feb.28 - Mar25) was 136,190 doses. In the first phase, Sinovac was the first vaccine administered to Thai people in the 1st lot for 200,000 doses and in the 2nd lot for 800,000 doses vaccinated the medical personnel and people in the high-risk and widespread areas. Subsequently, 117,600 doses of AstraZeneca vaccine were administered as supplement to the people age 60-years-old or older, healthcare providers, health volunteers, first responders and people in the provinces administered with Sinovac vaccine. When more vaccines are added in June, they will be administered to all age groups according to the next vaccination plan (Hfocus, 2021). On March 25th, 2021, fda opened a special channel to register the Johnson & Johnson’s covid-19 vaccine to expand immunization options for Thai people. The decision to take or not to take vaccine of healthcare providers affects the advice given to other groups of people. For this reason, the researcher interested in studying the group of nurses who are healthcare providers willing to receive the covid-19 vaccine the least to study the factors affecting the behavior for acceptance and uptake of the covid-19 vaccine in order to solve problems and create incentives for the willingness in the acceptance and uptake of the covid-19 vaccine. This will give the general public confidence and make the covid-19 vaccination in Thailand done quickly and effectively.
Literature Review
Barriers and enablers to vaccination :research efforts have also generated potentially effective strategies to improve vaccine acceptance and uptake which go beyond traditional information campaigns aspiring to change behaviors by improving knowledge, information on its own has shown a limited impact on facilitating vaccination uptake, but adding other strategies - such as reducing barriers; 1) using reminders, 2) planning prompts, 3) and training and building confidence in health workers 4,5) - has been shown to be effective (WHO, 2020). The emphasis on the confidence of healthcare providers in accepting vaccines is essential in creating strategies to overcome the vaccine acceptance barriers. Given the limited supply in the short to medium term, vaccines are likely to be prioritized for health workers at high risk of acquiring or transmitting base on the framework developed by the WHO Strategic Advisory Group of Experts on Immunization. (WHO Sage, 2020)
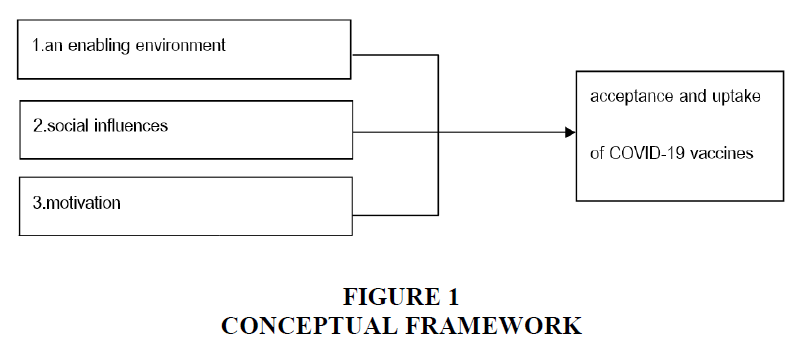
Drivers of Vaccine Uptake: Behavioral research identifies three categories of drivers of vaccine uptake, in addition to people having the necessary knowledge; 1) an enabling environment, 2) social influences, and 3) motivation. (WHO, 2020) Multiple groups influence uptake of vaccination, including political decision-makers, immunization program managers, community and religious leaders, health workers. These actors can facilitate or discourse vaccination by creating more or less enabling environments. It is important to consider how the behaviors off actors in the system might influence the behaviors of the general population.
1) An Enabling Environment: In light of these factors, there several ways to create enabling environments for encouraging widespread vaccination. In the current pandemic where people have indicated concerns about seeking health services due to fear of contracting COVID-19 in health facilities. An enabling environment is necessary and likely to increase acceptance and uptake of vaccination. But it should be accompanied by targeted, credible and clear communication from trusts sources demonstrating that getting vaccinated is important, in addition to ensuring that health care and community workers are well trained and well supported (WHO European Region, 2020). Environmental Factors might involve; 1. Location, 2. Cost, 3. Time, 4. The quality of the experience of being vaccinated, 5. Information, 6. The default, 7. Health regulations or mandates.
2) Social Influences: Sometimes, barriers to vaccine acceptance and uptake are the product of unfavorable social influences and/or insufficiently favorable ones. Such influences can include beliefs about what others in one's social do, or what they approve and disapprove. (Cialdini et al., 2006) Vaccination decision - making is also influenced by people's social networks, which include family members, friends, health professionals. Health professionals have more opportunities to influence vaccination behavior; can lead to greater impact of behavior change efforts. Social influences can be used to promote favorable behaviors of both health professionals and the general population. (Kim et al., 2015) Social Influences has 5 strategies to harness social influences are 1. Making social norms in favor of vaccination more salient 2. Highlighting new and emerging norms in favor of vaccination 3. Leveraging the role of health professionals 4. Supporting health professionals to promote vaccination 5. Amplifying endorsements from trusted community members.
3) Motivation: Vaccine acceptance and uptake may also be undermined by COVIV-19 vaccines being not fully effective, there are individual and group differences; some may be hesitant toward vaccination due to beliefs that have low-risk infection, other may have concerns about of safety of vaccines, while others may be hesitant because of religious values or lack of trust in the trust in the health system. (Larson HJ, 2011) Strategies to motivational barriers to vaccine acceptance and uptake 1) building timely trust in vaccines, 2) leveraging anticipated regret in communications, 3) emphasizing the social benefits of vaccination.
Conceptual framework
According to the research reviews and related articles, they can be summarized and used as the research conceptual framework as follows (Figure 1):
Research Methodology
Research Methodologies: This is a Descriptive Research
Population and studied samples
Population was the registered nurses residing in Thailand with unknown population size.
Sampling methods
The researcher used probability sampling selection using a simple random sampling method because there was a chance that the population would be selected equally (Donald & Pamela, 2010). The total number of samples was distributed with the questionnaires to collect the data in complete number. The complete samples were collected for further research.
Sample size
The researcher used Probability Sampling Techniques in the unknown population size. The estimated error was determined and set that the error was not greater than 0.05% at the 95% confidence level. The value was obtained from a sample at 400 from Taro Yamane’s table (Prakayrat & Amornwit, 2012).
Data collection
Since there was a chance the population was equally selected; the researcher collected the data from the random sampling by distributing questionnaires online to registered nurses. The data was collected after the questionnaires had passed the IOC (Index of item objective congruence) and had Cronbach’s Alpha=0.837. Before the questionnaires were collected, the researcher would go through the process of clarifying the data with the study participants and obtaining their consent to participate in the research beforehand.
Data analysis
The statistics used in the analysis were Percentage, Mean and t-test, Pearson Correlation and Multiple Regression to test the hypotheses of correlation coefficient.
Research Results
In terms of environmental factors affecting acceptance and uptake of COVID-19 vaccination: the priorities were ranked from the highest to the lowest means as follows; 1. Getting vaccinated influenced some of the needs such as traveling abroad and caring for the elderly, 2. Obtaining information about vaccines, pros, cons and side effects of each vaccine, 3. The workplace give the opportunity to decide whether to get vaccinated or not, 4. Quality of vaccine based on the information gained from experience of previous vaccine recipients, 5. The vaccination sites were near and convenient to commute, 6. Time to get vaccinated, waiting time, difficulty accessing vaccines, 7. Total vaccination cost such as cost of vaccine, travel expenses, work opportunity cost. The mean values were 4.58, 4.57, 4.54, 4.46, 4.45, 4.19 and 3.99, respectively.
The social influencing factors affecting the acceptance and uptake of COVID-19 vaccine: the priorities were ranked from the highest to the lowest means as follows; 1. Suggestions from leaders, experts and people you trust, 2. Getting advice from vaccinated healthcare providers, 3. Results of the vaccine responding to expectations of the healthcare sector, 4. Social environment emphasized on supporting vaccination, 5. Social norms / values where the population reside e on vaccination acceptance. The mean values were 4.46, 4.36, 4.24, 4.20, and 3.83, respectively.
Motivation factors affecting acceptance and uptake to COVID-19 vaccine: the priorities were ranked from the highest to the lowest means as follows; 1. Being communicated on the disadvantages of opportunity cost in order to get vaccinated, 2. Establishing trust in vaccines to be received prior to vaccination, 3. Being motivated by the benefits from vaccination. The mean values were 4.57, 4.48 and 4.44, respectively.
Hypothesis Test Results
Table 1 represents the correlation analysis using Pearson Correlation of rights to choose the type of COVID-19 vaccine and the acceptance and vaccination among nurses in Thailand.
| Table 1 Correlation Analysis Using Pearson Correlation | ||
| Correlations | Rights to choose the type of COVID-19 vaccine | |
| Acceptance and uptake of COVID-19 vaccine | Pearson Correlation | 0.066 |
| Sig. (2-tailed) | 0.187 | |
| N | 400 | |
According to Table 1, the research result revealed that the rights to choose the type of COVID- 91 vaccine did not affect the decision to be vaccinated at the statistical significance at 0.05.
Table 2 represents the correlation analysis using Multiple Regression by selecting Stepwise on the acceptance and vaccination among nurses in Thailand.
| Table 2 Correlation Analysis Using Multiple Regression | |||||
| Coefficientsa | Unstandardized Coefficients | Standardized Coefficients | |||
| B | Std. Error | Beta | t | Sig. | |
| (Constant) | 2.297 | 0.324 | 7.084 | 0 | |
| social influences | 0.248 | 0.072 | 0.201 | 3.425 | .001* |
| an enabling environment | 0.191 | 0.086 | 0.129 | 2.204 | .028* |
According to Table 2, the research result revealed that the social influences factor and an enabling environment factor influenced the decision on the acceptance and vaccination among nurses in Thailand.
The multiple linear regression equation estimated from this study was R2=0.087, which means such independent variable had little influence on the acceptance and vaccination decisions of nurses in Thailand at 8.7%. By using correlation analysis, the equation for the acceptance and vaccination decision of nurses in Thailand could be summarized as follows:
YAcceptance and vaccination = 2.297 + 0.248social influences factor + 0.191 an enabling environment factor
Table 3 represents an analysis on the level of acceptance behavior and uptake of COVID-19 vaccine among nurses in Thailand.
| Table 3 Analysis on the Level of Acceptance Behaviour | ||||||
| One-Sample Test | Test Value = 4.20 | |||||
| The level of acceptance behavior and | N | Mean | Std. Deviation | t | df | Sig. (2-tailed) |
| vaccination for COVIC-19 among nurses in Thailand | 400 | 4.1788 | 0.79467 | 0.535 | 399 | 0.593 |
According to Table 3, the research result revealed that the acceptance behavior and uptake of COVID-19 vaccine among nurses in Thailand was at the high level at the significance of 0.05 with the mean of 4.18.
Discussion and Conclusion
The acceptance behavior and vaccination among Thai nurses in Thailand revealed that having the rights to choose the type of COVID -19 vaccines did not affect their decision to get vaccinated at the statistical significance level of 0.05. The independent variable influenced the decision of acceptance and vaccination of nurses in Thailand with little influence of 8.7%. The social influences factor and an enabling environment factor were influencing factors for 0.248 and 0,191, respectively. These are inconsistent with the WHO’s behavioral research finding that three factors affecting the vaccination, which are 1. An enabling environment, 2. Social influences, and 3. Motivation (WHO, 2020). As the sample group was registered nurses with medical knowledge, they had greater confidence in their own decision-making rather than influences from other factors. They are also required to provide detailed, complete and easy-to-understand health information to the patients (Viroj, 2009, Urairak et al., 2017). The professional nursing has a good understanding on the concepts that influence researches. Nursing researchers often use a combination of quantitative and qualitative research methods. Therefore, it is likely that there is a confidence in the research results of vaccines that meet international standards (Siriporn, 2012). This is inconsistent with the survey data showing that professional nursing is the least willing to receive the vaccine for 47% (HITAP, 2021). Therefore, the researcher continued to test the level of acceptance and vaccination among nurses in Thailand. The results showed that the level of acceptance behavior and vaccination for COVID-19 among nurses in Thailand was high at the significance level of 0.05 with the mean of 4.18. The survey was conducted during the time when the vaccine data was insufficient to make the decision. After testing the hypothesis approximately 4months after the initial survey, the study found that the levels of acceptance and uptake of COVID-19 among nurses in Thailand were high. It was consistent with the research finding that there was more supporting information on vaccine, and the increasing numbers of people vaccinated without severe side effects worldwide. Factors influencing vaccine acceptance depended on the level of trust in the information communicated by the government (Guidry et al., 2021). Most Americans are willing to be vaccinated with the exception of at-risk groups (Kelly et al., 2021). Healthcare providers were identified as prime vaccination targets. The goal was set for vaccine acceptance in France. Nurses were less likely to receive vaccines than doctors. There is reluctance to receive vaccine is declining when greater acceptance of vaccine is rising (Gagneux-Brunon et al., 2021). Professional nurses are competent in a wide range of areas including continuous self-improvement competencies, higher education level, leadership, professional work and academic competency (Siriporn, 2012, Wong et al., 2021). For the side effects and duration of vaccine action, the research certifying vaccine is important to nurses in order to increase their acceptance of the vaccine (Kwok et al., 2021). Studying the willingness to accept the vaccine among healthcare providers in Taiwan and the formulation of policy to provide transparent information on vaccine will positively influence the successful vaccination (Kukreti et al., 2021). More than 95% of healthcare providers in Asia are willing to receive vaccines because of the awareness of the safety of vaccine, the quality assurance agency’s vaccine certification. The awareness of low-risk vaccine is an important strategy for vaccine acceptance (Chew et al., 2021, Yurttas et al., 2021, Ruiz & Bell, 2021). Keeping healthcare providers in good health through vaccination is the key element in vaccine acceptance (Wang et al., 2020). The family, friends and healthcare providers opinions correlate with the population’s willingness to be vaccinated (Cordina & Lauri, 2021). The general public is aware of the need for vaccination from the awareness measures among medical professionals. Therefore, with the recommendation of this research, Thailand should expedite the adequate vaccine acquirements and urgently get all healthcare professionals vaccinated to build credibility to the general public and ready to receive vaccination throughout the country. This will lead to the quick and effective solution to this crisis.
References
- Yurttas, B., Poyraz, B.C., Sut, N., Ozdede, A., Oztas, M., Ugurlu, S., Tabak, F., Hamuryudan, V., & Seyahi, E. (2021). Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: a web-based survey. Rheumatology International, 41(6), 1105-1114.
- Pfefferbaum, B., & North, C.S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510-512.
- Brewer, N.T., Chapman, G.B., Rothman, A.J., Leask, J., & Kempe, A. (2018). Understanding and increasing vaccination behaviors: Putting psychology into action. Psychological Science in the Public Interest, 18, 149-207.
- Kelly, B.J., Southwell, B.G., McCormack, L.A., Bann, C.M., MacDonald, P.D., Frasier, A.M., Bevc, C.A., Brewer, N.T., & Squiers, L. B. (2021). Predictors of willingness to get a COVID-19 vaccine in the US. BMC Infectious Diseases, 21(1), 1-7.
- Urairak, B., & Chaleoykitti, S. (2017). A model to manage the intention to stay in the nurse profession of nurse students at the army nursing college. PSUKU International Journal of Interdisciplinary Research (PSAKUIJIR), 6(1).
- Cialdini, R.B., Demaine, L.J., Sagarin, B.J., Barrett, D.W., Rhoads, K., & Winter, P.L. (2006). Managing social norms for persuasive impact. Social Influence, 1(1), 3-15.
- Kim, D.A., Hwong, A.R., Stafford, D., Hughes, D.A., O'Malley, A.J., Fowler, J.H., & Christakis, N.A. (2015). Social network targeting to maximise population behaviour change: a cluster randomised controlled trial. The Lancet, 386(9989), 145-153.
- Donald, R., & Pamela, S. (2010). Business research methods. (11th Edition). McGraw Hill: New York.
- Gagneux-Brunon, A., Detoc, M., Bruel, S., Tardy, B., Rozaire, O., Frappe, P., & Botelho-Nevers, E. (2021). Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. Journal of Hospital Infection, 108, 168-173.
- Health Intervention and Technology Assessment Program (HITAP). (2021). Opinions Survey of healthcare and public health personnel on getting COVIC-19 vaccine in Thailand. Retrieved March 28, 2021, from
- https://prachatai.com/journal/2021/02/91795
- Hfocus. (2021). Sinovac vaccines 800,000 doses has arrived in Thailand. Retrieved March 27, 2021, from https://www.hfocus.org/content/2021/03/21257
- Ruiz, J.B., & Bell, R.A. (2021). Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine, 39(7), 1080-1086.
- Retrieved March 27, 2021, from https://pubmed.ncbi.nlm.nih.gov/33461833/Vaccine.
- Guidry, J.P., Laestadius, L.I., Vraga, E.K., Miller, C.A., Perrin, P.B., Burton, C.W., Ryan, M., Fuemmeler, B.F., & Carlyle, K.E. (2021). Willingness to get the COVID-19 vaccine with and without emergency use authorization. American Journal of Infection Control, 49(2), 137-142.
- Wang, K., Wong, E.L.Y., Ho, K.F., Cheung, A.W.L., Chan, E.Y.Y., Yeoh, E.K., & Wong, S.Y.S. (2020). Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine, 38(45), 7049-7056.
- Kwok, K.O., Li, K.K., Wei, W.I., Tang, A., Wong, S.Y.S., & Lee, S.S. (2021). Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. International Journal of Nursing Studies, 114, 103854.
- Lazarus, J.V., Ratzan, S.C., Palayew, A., Gostin, L.O., Larson, H.J., Rabin, K., Kimball, S., & El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature medicine, 27(2), 225-228.
- Wong, L.P., Alias, H., Wong, P.F., Lee, H.Y., & AbuBakar, S. (2020). The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human vaccines & immunotherapeutics, 16(9), 2204-2214.
- Cordina, M., & Lauri, M.A. (2021). Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharmacy Practice (Granada), 19(1).
- Chew, N.W., Cheong, C., Kong, G., Phua, K., Ngiam, J.N., Tan, B.Y., Han, X., & Sharma, V.K. (2021). An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. International Journal of Infectious Diseases, 106, 52-60.
- Bunyavejchewin, P., & Sirichuanjun, K. (2021). How regime type and governance quality affect policy responses to COVID-19: A preliminary analysis. Heliyon, 7(2), e06349.
- Prakayrat, S., & Amornwit, W. (2012). Researching and analyzing data with a program SPSS version 20. SE-EDUCATION Public Company Limited: Bangkok.
- Kukreti, S., Lu, M.Y., Lin, Y.H., Strong, C., Lin, C.Y., Ko, N.Y., Chen, P.L., & Ko, W.C. (2021). Willingness of Taiwan’s healthcare workers and outpatients to vaccinate against COVID-19 during a period without community outbreaks. Vaccines, 9(3), 246.
- Kaur, S.P., & Gupta, V. (2020). COVID-19 Vaccine: A comprehensive status report. Virus research, 198114.
- Siriporn, C. (2012). Qualitative study in nursing. Wittayaphat. Co., Ltd: Bangkok.
- Le, T.T., Andreadakis, Z., Kumar, A., Román, R.G., Tollefsen, S., Saville, M., & Mayhew, S. (2020). The COVID-19 vaccine development landscape. Nat Rev Drug Discov, 19(5), 305-306.
- Viroj, W. (2009). Nursing Management to enhance quality in research departments. Chulalongkorn University Printing House : Bangkok.
- WHO European Region. (2020). Strategic considerations in preparing for development of COVID-19 vaccine and vaccination in the WHO European Region, Copenhagen. Retrieved March 28, 2021, from http://apps.who.int/iris/handle/10665/335940
- World Health Organization. (2020). Behavioural Considerations for Acceptance and Uptake of COVID-19 Vaccines. Retrieved from https://www.who.int/publications/i/item/9789240016927
- WHO Sage. (2020). WHO SAGE values framework for the allocation and prioritization of COVID - 19 vaccination. Retrieved from http://apps.who.int/iris/handle/10665/334299