Review Article: 2024 Vol: 28 Issue: 1
Development of Self-constructed Tool to Measure Factors Influencing Patient Empowerment through Online Patient Support Groups
Vivek Pandey, Sikkim Manipal University
Saibal Kumar Saha, Christ University
Samrat Kumar Mukherjee, Sikkim Manipal University
Ajeya Jha, Sikkim Manipal University
Citation Information: Pandey, V., Kumar Saha, S., Mukherjee, S.K., & Jha, A. (2024). Development of self-constructed tool to measure factors influencing patient empowerment through online patient support groups. Academy of Marketing Studies Journal, 28(1), 1-12.
Abstract
Objective: Numerous healthcare organizations offer Online Patient Support Groups (OPSGs) as a component of their comprehensive patient support services. The primary aim of establishing and maintaining these OPSGs is to provide patients with information and support. This research investigates the comparative influence of specific functions within OPSGs: Perceived Empathy, Information seeking, Perceived Social Support, and Homophily. Design: The objective of this study is to examine the effects of different factors within OPSGs, including the effectiveness of information seeking, perceived social support, perceived empathy, and homophily. Measurement: Data was gathered from participants of online health communities through a web-based survey. The collected data was analysed using the 16th edition of SPSS and AMOS version 26. Both exploratory and confirmatory factor analyses were conducted to examine the data. Results: 25 variables resulted in 5 latent constructs, and confirmatory factor analysis was conducted. The successful emergence of Online Patient Support Groups indicates that these fulfil the essential latent needs of patients.
Keywords
Online Patient Support Groups (OPSGs), Homophily, Perceived Social Support, Perceived Empathy, Online Health Communities, Patient Empowerment, Health care organizations, Online Health Communities.
Introduction
Knowledge sharing has been revolutionized due to the Internet, leading to the deprofessionalization of medicine, and giving greater power to health consumers. Those who are ill increasingly turn to the internet to find information about their condition. This easy access to information has resulted in a shift towards searching the Internet for advice before consulting healthcare professionals. The use of Online Health Information (OHI) to make healthcare decisions includes seeking medical care, adhering to treatment plans, managing health changes, engaging in discussions with health professionals, changing health behaviours, and providing social support (Pluye et al., 2019). This use of OHI can empower consumers to take control of their health and contribute to positive health outcomes . The COVID pandemic has accelerated this trend towards increased access and use of internet based health information (Thapa et al., 2021).
Online health communities provide a space for individuals with similar medical conditions to offer guidance, seek support, and gain knowledge from one another. In today's Web 2.0 era, social media is heavily integrated into people's daily lives, impacting their health behaviour (Mukherjee et al., 2019). The ability to access information on social media platforms has revolutionized traditional information retrieval methods through search engines.
The swift expansion of social media is transforming communication, interaction, and cooperation among individuals, businesses, and government. It has become an essential element of everyday life for people worldwide. With Facebook alone having more than 2 billion users and nearly 70 percent of all internet users participating in some form of social media (Sharma & Khadka, 2019), this technological tool now offers patients a fresh way to share health related information. Social media and healthcare intersections have transformed how healthcare consumers manage their health needs.
Literature Review
Online Patient Support Groups
Online Patient Support Groups (OPSGs) are virtual platforms where individuals convene to discuss a health issue (Young & Miller, 2019). Most of these platforms comprise patients or people undergoing a medical issue and can be isolated sites or sub forums within a more extensive site or service, such as Reddit or Facebook (Hinson, 2017). Through OPSGs, patients can obtain and disseminate disease information to others who may relate to their experience.
OPSG members can access various support networks and information on various health topics at an affordable cost. Users do not expect to receive any monetary compensation or returns for sharing these valuable resources and services (Mirzaei & Esmaeilzadeh, 2021). An online patient support group is a collection of individuals who share the same experiences and worries, offering each other emotional and moral support. These groups serve various purposes, such as educating patients and their families, exchanging disease related experiences, empowering members, raising public awareness, and generating funds. OPSGs offer a more efficient solution for those struggling with medical conditions as it relies on social connection and support among people facing similar challenges. OPSGs (OPSGs) can offer patients suffering from chronic diseases, particularly lifestyle related diseases such as obesity, type 2 diabetes, or cancer, valuable knowledge from their peers, emotional support, and help them improve their self care. By sharing anecdotal information, OPSGs assist patients in attaining a more positive emotional outlook toward chronic diseases, motivating them to participate in the community's activities (Rezaei et al., 2020). The main goal of the majority of OPSGs is to offer patients a platform to connect, interact and seek emotional support from one another while managing their disease and care. Through OPSGs, patients engage in additional activities that enhance the value of patient provider interactions.
Perceived Social Support
When it comes to healthcare, the primary reason patients use OPSGs is for social support. Social support refers to interactions within relationships that aim to enhance coping, self esteem, a sense of belonging, and personal competence through exchanges of psychosocial resources. Multiple pathways link social relationships and well being, which is encapsulated by the concept of social support and has been shown to positively affect mental health, work related stress, and resilience. The OPSGs create a positive community of individuals united by shared interests, without being limited by physical distance, where they discuss their questions and celebrate achievements in a welcoming and supportive environment. The fundamental principle of social support suggests that individuals with stress seek solace in their social circles and close relationships, where they can discuss their problems and receive various forms of support, including informational, emotional, esteem, and instrumental support.
When peer patients exhibit a high level of empathy towards an individual's health condition and offer support in a caring manner, patients may interpret this interaction as social support. Studies have shown that social support is a crucial psychosocial coping mechanism that people rely on to combat severe mental health issues and sustain their subjective well being (Qi et al., 2020). How individuals perceive social support, or the feeling of being supported by others, is significant in their resilience and well being. Studies in psychology have indicated that the perception of social support can prevent adverse effects such as stress, anxiety, and depression while promoting positive effects such as happiness (Sato et al., 2020). There are generally two interpretations of social support: perceived social support and received social support. Perceived social support is an individual's subjective evaluation of the availability of friends and family members to provide material, psychological, and general support during challenging times, while receiving support refers to the actual support an individual receives from their social network (Eagle et al., 2019).
Perceived Social support is a crucial element of well being, characterized by individuals showing concern, respect, and support towards each other as part of a social network. Lower morbidity and mortality rates have been observed in individuals with social support. Additionally, social support has been found to reduce psychological distress and adjust chronic stress states, thereby contributing to psychological adjustment (Yang et al., 2022).
Homophily
Homophily refers to an individual's tendency to build connections and form stronger bonds with those with similar features or characteristics (Miller et al.,2019). People who use OPSGs frequently cite a sense of universality, comfort in knowing that others share their experiences and emotions, and a sense of similarity and connection with those going through similar situations or conditions as the main reasons for participating in OPSGs. (Kashian and Jacobson, 2020).
In research on friendship conducted, the term "homophily" was first used to describe the tendency for people with similar features or characteristics to create close bonds (Berry et al., 2018). The homophily idea states that people are more inclined to interact or engage with those with comparable behaviours, qualities, or features. The research infers that homophily should be viewed as a dynamic and ever changing human trait rather than a fixed or static feature. The study also proposes that stakeholders take advantage of the intricate nature of users' homophilic behaviours in online social networking sites to address pertinent social issues.
Based on the homophily theory, communication between individuals is more likely to occur when they share similarities. When people are surrounded by others who are like them, it can increase their level of comfort in different situations. In the context of online support groups, homophily has been shown to improve members' satisfaction with their interactions in the group. Sharing experiences related to diseases and treatment protocols is a crucial element of online health community discussions. Therefore, we propose that when patients perceive a sense of homophily with other patients, it can enhance the effectiveness of information seeking and social support, leading to greater perceived empathy.
Perceived Empathy
The ability to understand and acknowledge the experiences and emotions of others, known as empathy, is an integral aspect of providing adequate support (Sharma et al., 2021). Additionally, quantitative evidence indicates a strong association between empathetic interactions and alleviating symptoms in mental health care (Elliot et al., 2018).
Patients who participate in OPSGs can discuss and express their experiences, emotions, and concerns related to their illness, and this disclosure behaviour prompts empathetic responses from fellow participants. The study indicated that patients in such groups share information regarding their illness and treatment and relay their emotional states and perceptions, which leads to reciprocal empathic reactions from other members. According to recent research in the healthcare sector, empathy emerges as a significant benefit of utilizing OPSGs (Medeiros & Bosse, 2016). This can support healing by reducing distress and increasing a positive outlook.
The way patients view empathy is essential in delivering care and has been proven to affect their health outcomes significantly. Perceived empathy refers to a patient's understanding of how fellow members, in terms of their compassion, kindness, authenticity, and understanding, respond to their shared health problems or stories in an online community.
Information Seeking
Healthcare systems and physician patient relationships are significantly impacted by health information seeking and communication between patients and physicians. Patients often resort to various sources to seek health information, both before and after visiting their physicians, which can impact patient trust in their doctors and the extent to which they comply with treatment (Apker et al., 2018). OPSGs (OPSGs) are a typical online platform for patients to gather health related information and connect with medical professionals. Patients can seek health related support and gather information by creating posts and communicating through online messages. These communities enable patients to self diagnose simple symptoms while maintaining their privacy. OPSGs facilitate swift and seamless access to healthcare related information for patients anytime, anywhere, using innovative technologies like smartphones, tablets, or other devices (Lu et al., 2021).
The relationship between a patient and physician can be positively impacted by searching for health information on the internet, but this outcome depends on the patient's communication of the information to the doctor and the existing rapport between them. For healthcare information services to succeed on the OPSGs, user participation is crucial in seeking health information and sharing that information with others (Li et al., 2018).
Patient Empowerment
OPSGs (OPSGs) can facilitate the process of self management by allowing patients to share health related information and experiences. This means that OPSGs can play an active role in engaging and empowering patients during their healthcare journey. Participation in the innovation of healthcare services allows healthcare organizations to take a proactive stance in creating and supporting successful methods for online value co creation. Empowering patients increase their participation in value cocreation, resulting in better outcomes (Rezaei et al., 2020). Empowerment allows individuals to perceive a stronger connection between their goals, effort, and success.
The idea of empowerment may refer to self assurance, power, independence, and self
reliance, depending on the social and cultural environment. At its most complete level, empowerment entails giving people the freedom and knowledge required to make decisions and take actions and the capacity to handle resources and make decisions that influence their life. OPSGs played a crucial role in empowering patients by allowing them to actively participate and have an equal voice in the patient provider interaction (Palumbo, 2017). They also assisted patients in overcoming psychological distress brought on by their medical diagnosis or bad encounters with their care. These personal experiences were critical to patient empowerment, and OPSGs offered a secure place for individuals to process them (Johansson et al., 2021). There is a universal consensus that a well educated patient is better able to make informed decisions, stick to therapy, reduce anxiety, and actively participate in their healthcare. This is especially important in chronic diseases when patients must undertake long term lifestyle changes and adapt to their situations.
In Table 1, OP is OPSGs, HP is Homophily, PSS is Perceived Social Support, PET is Patient Empowerment, PE is Perceived Empathy, and IS is Information Seeking Effectiveness.
| Table 1 Description Of Variables |
||
|---|---|---|
| Sl. No | Variable | Description |
| 1 | OP1 | To search for Information that can improve my health |
| 2 | OP2 | To read about other people's experiences of disease/ bad health/ a Treatment |
| 3 | OP3 | To be able to make more well-informed decisions regarding my health |
| 4 | OP4 | To search for compassion when I am not feeling well |
| 5 | OP5 | To get feedback from others who have had the same health problem as I have |
| 6 | HP1 | Do not think like me/ Think like me |
| 7 | HP2 | Do not behave like me/ Behave like me |
| 8 | HP3 | Have a health situation different from mine/ Have a health situation like mine |
| 9 | HP4 | Does not share my emotion/ Shares my emotion |
| 10 | HP5 | Are unlike me/ Are like me |
| 11 | PSS1 | I knew a friend on the discussion board with whom I could share my joys and sorrows. |
| 12 | PSS2 | I got the emotional help and support that I needed from OPSGs |
| 13 | PSS3 | I can count on my friends of OPSGs when things go wrong |
| 14 | PSS4 | I knew a special friend on the discussion board who has been a real source of comfort to me |
| 15 | PSS5 | The online patient support group is willing to help me make decisions |
| 16 | PE1 | Unsympathetic/ Sympathetic |
| 17 | PE2 | Not Supportive/ Supportive |
| 18 | PE3 | Insincere/ Sincere |
| 19 | PE4 | Serious/ Carefree |
| 20 | PE5 | Not Compassionate/ Compassionate |
| 21 | IS1 | To obtain readily usable information |
| 22 | IS2 | To obtain credible information |
| 23 | IS3 | To obtain relevant information |
| 24 | IS4 | To obtain reliable information |
| 25 | IS5 | To obtain information promptly |
Methodology
A cross sectional survey was carried out with individuals from different regions of the world between April 2020 and September 2021. This survey used convenience sampling, and 820 answers were received. Out of these, 700 replies were selected, and the remaining 120 were disqualified for reasons such as incompleteness, lack of use of OPSGs for medical advice, preference for in person help, or need for sympathy and support. Selecting a questionnaire is a suitable method for comprehending patients' opinions regarding OPSGs. The responses to the questionnaire were evaluated using a 7 point Likert scale (7= Strongly Disagree, 6= Disagree, 5= More or Less Agree, 4= Undecided, 3= More or Less Agree, 2= Agree, 1= Strongly Agree), Usage of OPSGs to seek Homophily and Perceived Empathy were scored using 7 point semantic differential scale. The survey was distributed to patients using various online platforms such as Instagram, Messenger, Facebook Support Groups, Online patient support group forums, Discussion boards, and websites. Since the survey was conducted online, patients from distant locations could also participate, making it a convenient data collection method. This approach reduced the researcher's effort, saved time, and lowered costs.
The questionnaire responses and categorical variables were converted into numerical codes using SPSS version 25.
Human Ethics: Participants in the study were provided with detailed information about the research and voluntarily filled out their forms. They were not coerced or compelled to participate and were free to withdraw their responses at any point during the study. Throughout the research, adequate measures were taken to ensure no misleading information or deceptive practices were employed.
The data collected from the survey were coded and analysed using the 16th version of SPSS. The purpose of the analysis was to gain insights into the perceptions and beliefs of patients using OPSGs.
EFA Exploratory factor analysis was done using SPSS version 16 with the help of the Principal Components method. The maximum iterations for convergence were 25. Rotation was performed with the help of the Promax method using Kappa value 4.
CFA Confirmatory factor analysis was performed using AMOS version 26 with the help of the Maximum Likelihood method (Saha et al., 2022).
Results
Table 2 shows the descriptive statistics of the variables taken for the study. The minimum value of the variables was 1, while the maximum value of the variables was 7. The skewness and kurtosis values of all the variables had acceptable limits of +1.5 and 1.5.
| Table 2 Descriptive Statistics |
||||||
|---|---|---|---|---|---|---|
| Sl.No. | Variable | Mean | Std. Deviation | Variance | Skewness | Kurtosis |
| 1 | OP1 | 3.96 | 1.701 | 2.894 | 0.027 | -0.833 |
| 2 | OP2 | 3.8 | 1.735 | 3.011 | 0.03 | -0.891 |
| 3 | OP3 | 4.12 | 1.733 | 3.003 | -0.064 | -0.937 |
| 4 | OP4 | 3.75 | 1.745 | 3.045 | 0.156 | -0.931 |
| 5 | OP5 | 3.96 | 1.701 | 2.894 | 0.027 | -0.833 |
| 6 | HP1 | 3.59 | 1.931 | 3.73 | 0.131 | -1.214 |
| 7 | HP2 | 3.91 | 2.003 | 4.012 | 0.083 | -1.28 |
| 8 | HP3 | 4.33 | 1.94 | 3.762 | -0.054 | -1.274 |
| 9 | HP4 | 3.97 | 1.981 | 3.925 | 0.059 | -1.262 |
| 10 | HP5 | 3.68 | 1.956 | 3.827 | 0.119 | -1.246 |
| 11 | PSS1 | 3.71 | 1.934 | 3.741 | 0.1 | -1.208 |
| 12 | PSS2 | 3.96 | 2.001 | 4.005 | -0.018 | -1.259 |
| 13 | PSS3 | 4.09 | 1.975 | 3.902 | -0.07 | -1.211 |
| 14 | PSS4 | 4.39 | 1.983 | 3.933 | -0.161 | -1.223 |
| 15 | PSS5 | 3.47 | 1.905 | 3.629 | 0.174 | -1.214 |
| 16 | PE1 | 3.89 | 1.967 | 3.871 | 0.1 | -1.25 |
| 17 | PE2 | 3.64 | 1.979 | 3.916 | 0.178 | -1.231 |
| 18 | PE3 | 4.11 | 1.953 | 3.815 | 0.038 | -1.237 |
| 19 | PE4 | 3.92 | 1.954 | 3.817 | 0.077 | -1.237 |
| 20 | PE5 | 3.51 | 1.91 | 3.647 | 0.188 | -1.176 |
| 21 | IS1 | 3.81 | 1.978 | 3.911 | 0.132 | -1.196 |
| 22 | IS2 | 3.37 | 1.911 | 3.652 | 0.33 | -1.068 |
| 23 | IS3 | 4.28 | 1.942 | 3.772 | -0.009 | -1.281 |
| 24 | IS4 | 4.51 | 1.925 | 3.707 | -0.278 | -1.12 |
| 25 | IS5 | 3.8 | 1.97 | 3.88 | 0.128 | -1.17 |
Table 3 shows the variance explained by the five factors obtained from the analysis. The variance explained by the individual factors ranges between 12.14% to 29.74%, while the total variance explained by all the factors is 91.04%.
| Table 3 Variance Explained |
||||||
|---|---|---|---|---|---|---|
| Component | Initial Eigenvalues | Extraction Sums of Squared Loadings | ||||
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 7.43 | 29.74 | 29.74 | 7.43 | 29.74 | 29.74 |
| 2 | 4.75 | 19.02 | 48.76 | 4.75 | 19.02 | 48.76 |
| 3 | 3.94 | 15.77 | 64.53 | 3.94 | 15.77 | 64.53 |
| 4 | 3.59 | 14.37 | 78.90 | 3.59 | 14.37 | 78.90 |
| 5 | 3.03 | 12.14 | 91.04 | 3.03 | 12.14 | 91.04 |
Table 4 shows the pattern matrix of the five factors obtained from the analysis. The variables PE1, PE2, PE3, PE4, and PE5 with factor loadings 0.993, 0.986, 0.979, 0.993, and 0.976 constitute the first factor named PE. Since these factor loadings are above 0.5 they can be considered to be constituting the latent factor PE (Saha, & Jha, 2023). As a result, the empathy and support those users got became a source of personal inspiration, allowing them to establish a new identity (Montali et al., 2022). Empathy is acknowledged as a crucial skill for healthcare practitioners, and patients experience various advantages when they receive empathetic treatment, such as enhanced pain management, better adherence to medication, and increased satisfaction with their care (Winter et al., 2022).
| Table 4 Pattern Matrix |
|||||
|---|---|---|---|---|---|
| Factors | |||||
| Variables | 1 | 2 | 3 | 4 | 5 |
| OP1 | 0.947 | ||||
| OP2 | 0.901 | ||||
| OP3 | 0.894 | ||||
| OP4 | 0.909 | ||||
| OP5 | 0.947 | ||||
| HP1 | 0.975 | ||||
| HP2 | 0.991 | ||||
| HP3 | 0.968 | ||||
| HP4 | 0.996 | ||||
| HP5 | 0.980 | ||||
| PSS1 | 0.541 | ||||
| PSS2 | 0.988 | ||||
| PSS3 | 0.986 | ||||
| PSS4 | 0.971 | ||||
| PSS5 | 0.979 | ||||
| PE1 | 0.993 | ||||
| PE2 | 0.986 | ||||
| PE3 | 0.979 | ||||
| PE4 | 0.993 | ||||
| PE5 | 0.976 | ||||
| IS1 | 0.991 | ||||
| IS2 | 0.965 | ||||
| IS3 | 0.970 | ||||
| IS4 | 0.921 | ||||
| IS5 | 0.990 | ||||
The variables HP1, HP2, HP3, HP4, and HP5 with factor loadings 0.975, 0.991, 0.968, 0.996, and 0.980 constitute the second factor termed HP. Homophily leads to uniformity within social networks, causing attributes that contribute to creating similar connections to cluster among groups of connected individuals. This tendency for homophily promotes the adoption and spread of behaviours, as people are more susceptible to being influenced by those who share similarities (Heaton & Gondal, 2023).
The variables IS1, IS2, IS3, IS4, and IS5 with factor loadings 0.991, 0.965, 0.970, 0.921, and 0.990 constitute the third factor termed IS. A direct association exists between seeking information and one's attitude and even intention toward engaging in health related behaviours. For example, individuals who actively searched for medical information on the Internet expressed stronger beliefs about their health than those who did not engage in such information seeking activities (Li & Zheng, 2022).
OP1, OP2, OP3, OP4, and OP5 with factor loadings 0.947, 0.901, 0.894, 0.909, and 0.947 constitute the fourth factor termed OP. Individuals experiencing health issues turn to OPSGs to seek assistance and guidance (Yang et al., 2019). OPSGs are adequate resources for engaging and inspiring patients due to their patient centred approach, ability to foster a sense of personal competence, facilitate meaningful community interaction, and empower individuals seeking help (Liu et al., 2018).
The variables PSS1, PSS2, PSS3, PSS4, and PSS5 with factor loadings 0.541, 0.988, 0.986, 0.971, and 0.979 constitute the fifth factor, PSS. Perceived social support refers to the understanding of being nurtured and cherished, respected and appreciated, and connected within social circles. It is crucial to note that the effectiveness of social support relies on the compatibility between the provider and recipient of support, meaning that individuals are more inclined to offer and receive social support when both parties share a common sense of social identity.
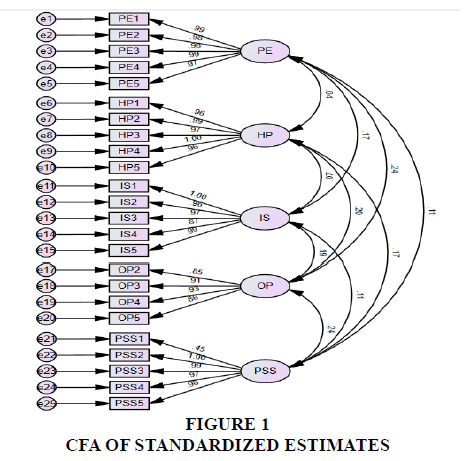
Figure 1 shows the diagrammatic representation of the standardized estimates of CFA of the various variables and their latent constructs. There is no correlation between PE and HP (0.04). Also, there is no correlation between HP and IS (0.07). Although there is some positive correlation between the other latent constructs, their magnitude is very low, ranging from 0.11 to 0.24. The factor loadings of the individual constructs are high, which justifies these variables to be a part of the latent constructs. Table 5 shows the regression weights of the variables along with their standard error, composite reliability, and p values. As the p values of each variable are significant and the standard error is less than 0.05, it can be inferred that the variables constitute well to the latent constructs.
| Table 5 Regression Weights |
||||||
|---|---|---|---|---|---|---|
| Estimate | S.E. | C.R. | P | |||
| PE1 | <--- | PE | 1 | |||
| PE2 | <--- | PE | 0.993 | 0.009 | 109.242 | *** |
| PE3 | <--- | PE | 0.979 | 0.009 | 107.55 | *** |
| PE4 | <--- | PE | 0.993 | 0.007 | 149.887 | *** |
| PE5 | <--- | PE | 0.946 | 0.01 | 90.115 | *** |
| HP1 | <--- | HP | 0.936 | 0.01 | 93.122 | *** |
| HP2 | <--- | HP | 1.001 | 0.005 | 208.183 | *** |
| HP3 | <--- | HP | 0.948 | 0.009 | 106.591 | *** |
| HP4 | <--- | HP | 1 | |||
| HP5 | <--- | HP | 0.951 | 0.01 | 97.597 | *** |
| IS1 | <--- | IS | 1 | |||
| IS2 | <--- | IS | 0.93 | 0.01 | 90.907 | *** |
| IS3 | <--- | IS | 0.951 | 0.01 | 100.11 | *** |
| IS4 | <--- | IS | 0.851 | 0.018 | 47.121 | *** |
| IS5 | <--- | IS | 0.99 | 0.005 | 202.953 | *** |
| OP2 | <--- | OP | 0.915 | 0.027 | 34.108 | *** |
| OP3 | <--- | OP | 0.974 | 0.024 | 40.022 | *** |
| OP4 | <--- | OP | 1 | |||
| OP5 | <--- | OP | 0.9 | 0.026 | 34.372 | *** |
| PSS1 | <--- | PSS | 0.441 | 0.033 | 13.431 | *** |
| PSS2 | <--- | PSS | 1 | |||
| PSS3 | <--- | PSS | 0.982 | 0.006 | 151.876 | *** |
| PSS4 | <--- | PSS | 0.967 | 0.01 | 100.103 | *** |
| PSS5 | <--- | PSS | 0.932 | 0.009 | 106.484 | *** |
Model Fit Indices: NFI = 0.814, TLI = 0.774, CFI = 0.818, RFI = 0.769
| Table 6 Validity Analysis |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| CR | AVE | MSV | MaxR(H) | PE | HP | IS | OP | PSS | |
| PE | 0.99 | 0.964 | 0.058 | 0.995 | 0.982 | ||||
| HP | 0.99 | 0.956 | 0.042 | 1.003 | 0.042 | 0.978 | |||
| IS | 0.98 | 0.921 | 0.036 | 0.999 | 0.171*** | 0.066† | 0.960 | ||
| OP | 0.93 | 0.787 | 0.058 | 0.943 | 0.241*** | 0.204*** | 0.190*** | 0.887 | |
| PSS | 0.954 | 0.814 | 0.057 | 0.995 | 0.114** | 0.165*** | 0.113** | 0.238*** | 0.902 |
Significance of Correlations:
† p < 0.100
* p < 0.050
** p < 0.010
*** p < 0.001
As shown in Table 6, the "Composite Reliability" (CR) was greater than 0.7, "Average Variance Extracted" (AVE) for all the variables was more than 0.5, and the "Maximum Shared Variance" (MSV) was smaller than Maximal Reliability (MaxR (H)). Thus, the model had no validity concerns (Saha & Jha, 2022).
Discussion
The objective of the present study has been to use exploratory and CFA to investigate the factorial structure of the specific functions within OPSGs, namely Perceived Empathy, Information seeking, Perceived Social Support, and Homophily. The EFA provides five distinct factors that explain over 91% of the variations. The first factor accounts for about 29% of variations. Looking into this, exploratory factor analysis provides clear evidence of the convergent and divergent validity of the scales.
Confirmatory factor analysis has been performed hereafter, and the goodness of fit indices such as NFI, TLI, CFI, and RFI reflects good fit, though marginally below the acceptable levels. This signifies a necessity for further exploration into the underlying factors impacting the factor structures.
Conclusion
Successful emergence of OPSGs indicates that these fulfil the critical latent needs of patients. In the traditional setup, highly vulnerable patients struggled for social, informational, emotional, and empathetic support. This has affected their self efficacy and autonomy also. Online patients support groups fulfil these unmet needs of patients. This study investigates the validity of scales for measuring Perceived Empathy, Information seeking, Perceived Social Support, and Homophily of individuals visiting OPSGs. Results indicate reasonably high goodness of fit indices, though still marginally below the accepted limits. The paper highlights the importance of socio emotional support, which is a part of the dynamics of OPSGs. It further emphasizes this to be the moral basis to encourage this trend. Although the socio emotional aspect of OPSGs has been known for some time, this paper still provides a firm basis to uphold this aspect, including patient empowerment.
This study has implications for future researchers. They need to explore the dimensions of these factors further to achieve better goodness of fit. Future researchers can also examine whether OPSGs bring about long term changes in patients' emotions. The study has limitations. Data has been collected online, and hence randomness has been compromised. It needs to explain the nonresponses. However, studies indicate that online data collection is comparable to offline surveys.
Finally, the research's online support group exemplifies how people adeptly use the available technology to negotiate, redefine, and reinvent pre existing socio emotional and informational codes to make sense of their illness experiences.
References
Apker, J., Baker, M., Shank, S., Hatten, K., & VanSweden, S. (2018). Optimizing hospitalist-patient communication: an observation study of medical encounter quality. The Joint Commission Journal on Quality and Patient Safety, 44(4), 196-203.
Indexed at, Google Scholar, Cross Ref
Berry, D. L., Blonquist, T. M., Pozzar, R., & Nayak, M. M. (2018). Understanding health decision making: An exploration of homophily. Social Science & Medicine, 214, 118-124.
Indexed at, Google Scholar, Cross Ref
Eagle, D. E., Hybels, C. F., & Proeschold-Bell, R. J. (2019). Perceived social support, received social support, and depression among clergy. Journal of Social and Personal Relationships, 36(7), 2055–2073.
Indexed at, Google Scholar, Cross Ref
Heaton, B., & Gondal, N. (2023). Health-based homophily in public housing developments. BMC Public Health, 23(1), 238.
Indexed at, Google Scholar, Cross Ref
Hinson, K. L. (2017). Framing illness through Facebook-enabled online support groups. Communication Design Quarterly Review, 4(2b), 22-31.
Johansson, V., Islind, A. S., Lindroth, T., Angenete, E., & Gellerstedt, M. (2021). Online communities as a driver for patient empowerment: Systematic review. Journal of medical Internet research, 23(2), e19910.
Li, J., & Zheng, H. (2022). Online Information Seeking and Disease Prevention Intent During COVID-19 Outbreak. Journalism & Mass Communication Quarterly, 99(1), 69–88.
Li, Y., Wang, X., Lin, X., & Hajli, M. (2018). Seeking and sharing health information on social media: A net valence model and cross-cultural comparison. Technological Forecasting and Social Change, 126, 28-40.
Liu, X., Sun, M., & Li, J. (2018). Research on gender differences in online health communities. International journal of medical informatics, 111, 172-181.
Lu, X., & Zhang, R. (2021). Impact of patient information behaviours in online health communities on patient compliance and the mediating role of patients' perceived empathy. Patient Education and Counseling, 104(1), 186-193.
Medeiros, L., Bosse, T. (2016). Empirical Analysis of Social Support Provided via Social Media. In: Spiro, E., Ahn, YY. (eds) Social Informatics. SocInfo 2016. Lecture Notes in Computer Science(), vol 10047. Springer, Cham.
Miller, J. J., Cooley, M., Niu, C., Segress, M., Fletcher, J., Bowman, K., & Littrell, L. (2019). Support, information seeking, and homophily in a virtual support group for adoptive parents: Impact on perceived empathy. Children and Youth Services Review, 101, 151-156.
Mirzaei, T., & Esmaeilzadeh, P. (2021). Engagement in online health communities: channel expansion and social exchanges. Information & Management, 58(1), 103404.
Montali, L., Zulato, E., Frigerio, A., Frangi, E., & Camussi, E. (2022). Mirroring, monitoring, modeling, belonging, and distancing: Psychosocial processes in an online support group of breast cancer patients. Journal of Community Psychology, 50(2), 992-1007.
Indexed at, Google Scholar, Cross Ref
Mukherjee, S. K., Kumar, J., Jha, A. K., & Rani, J. R. (2019). Role of Social Media Promotion of Prescription Drugs on Patient Belief-system and Behaviour. International Journal of e-Collaboration (IJeC), 15(2), 23-43.
Indexed at, Google Scholar, Cross Ref
Palumbo, R. (2017). The bright side and the dark side of patient empowerment: Cocreation and co-destruction of value in the healthcare environment. Springer.
Pluye, P., El Sherif, R., Granikov, V., Hong, Q. N., Vedel, I., Galvao, M. C. B., ... & Grad, R. (2019). Health outcomes of online consumer health information: A systematic mixed studies review with framework synthesis. Journal of the Association for Information Science and Technology, 70(7), 643-659.
Indexed at, Google Scholar, Cross Ref
Qi, M., Zhou, S. J., Guo, Z. C., Zhang, L. G., Min, H. J., Li, X. M., & Chen, J. X. (2020). The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. Journal of Adolescent Health, 67(4), 514-518.
Indexed at, Google Scholar, Cross Ref
Rezaei Aghdam A, Watson J, Cliff C, Miah S. Improving the Theoretical Understanding Toward Patient-Driven Health Care Innovation Through Online Value Cocreation: Systematic Review. J Med Internet Res 2020;22(4):e16324.
Indexed at, Google Scholar, Cross Ref
Saha, S. K. & Jha, A., (2023). Correlation Between Evaluative Beliefs of Patients, Reminder and Medication Adherence. International Journal of Asian Business and Information Management (IJABIM), 13(1), 1-16.
Indexed at, Google Scholar, Cross Ref
Saha, S. K., & Jha, A. (2022). IMPACT OF REMINDER ON MEDICATION ADHERENCE: A STRUCTURAL EQUATION MODEL, BASED ON STUDY IN SIKKIM, INDIA. Bioscience Journal, 38.
Indexed at, Google Scholar, Cross Ref
Saha, S. K., Adhikary, A., & Jha, A. (2022). Enhancement in medication adherence amidst COVID-19 using active reminders. The European Physical Journal Special Topics, 231(18-20), 3497-3504.
Indexed at, Google Scholar, Cross Ref
Sato, W., Kochiyama, T., Uono, S. et al. Amygdala activity related to perceived social support. Sci Rep 10, 2951 (2020).
Sharma, A., Lin, I. W., Miner, A. S., Atkins, D. C., & Althoff, T. (2021, April). Towards facilitating empathic conversations in online mental health support: A reinforcement learning approach. In Proceedings of the Web Conference 2021 (pp. 194-205).
Indexed at, Google Scholar, Cross Ref
Sharma, S. and Khadka, A. (2019), "Role of empowerment and sense of community on online social health support group", Information Technology & People, Vol. 32 No. 6, pp. 1564-1590.
Indexed at, Google Scholar, Cross Ref
Thapa, D. K., Visentin, D. C., Kornhaber, R., West, S., & Cleary, M. (2021). The influence of online health information on health decisions: A systematic review. Patient Education and Counseling, 104(4), 770-784.
Indexed at, Google Scholar, Cross Ref
Winter, R., Leanage, N., Roberts, N., Norman, R. I., & Howick, J. (2022). Experiences of empathy training in healthcare: A systematic review of qualitative studies. Patient Education and Counseling.
Indexed at, Google Scholar, Cross Ref
Yang Q, Kanjanarat P, Wongpakaran T, Ruengorn C, Awiphan R, Nochaiwong S, Wongpakaran N, Wedding D. Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support. Healthcare. 2022; 10(5):812.
Indexed at, Google Scholar, Cross Ref
Yang, D., Yao, Z., Seering, J., & Kraut, R. (2019). The channel matters: Self-disclosure, reciprocity, and social support in online cancer support groups. In Proceedings of the 2019 chi conference on human factors in computing systems (pp. 1-15).
Indexed at, Google Scholar, Cross Ref
Young, A. L., & Miller, A. D. (2019, May). "This Girl is on Fire" Sensemaking in an Online Health Community for Vulvodynia. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems (pp. 1-13).
Indexed at, Google Scholar, Cross Ref
Received: 31 Jul 2023, Manuscript No. AMSJ 23 13838; Editor assigned: 01 Aug 2023, PreQC No. AMSJ 23 13838(PQ); Reviewed: 29 Sep 2023, QC No. AMSJ 23 13838; Revised: 19 Oct 2023, Manuscript No. AMSJ 23 13838R); Published: 21 Nov 2023