Research Article: 2021 Vol: 25 Issue: 2
Enhancing Service Engagement and Collaborative Decision Making Through Wearable Device Adoption
Vaidik Bhatt, ICFAI Business School, IFHE University
Samyadip Chakraborty, ICFAI Business School, IFHE University
Abstract
With the aid of IoT (Internet of Things) powered wearable sensors, it is possible to measure the pulse, blood pressure, and other body functions by the physicians in real-time. The study highlighted that use of wearable tracker eventually leads to improved health for patients through improved medical service engagement. Survey-based approach was implemented to collect primary data from 131 respondents using wearable devices. The statistics were evaluated using partial least squares-structural equation modeling (PLS-SEM) approach with smartPLS 3.0 software. The results revealed that information pervasiveness has no major effect on collaborative decision making, However, Patient-Provider interaction are found to be positively impacting collaborative decision-making. Key outcome came out to be an important finding as collaborative decisions did not exert significant impact on service engagement.
Keywords
Healthcare; Service Engagement; patient-Provider Interaction; Collaborative Decision making; Internet of Things; Information Pervasiveness; Wearable Health Devices; PLS-SEM.
Introduction
Unlike any other industry, healthcare as a promising sector is also using the technological progressions to generate competitive advantage. Healthcare transformed itself by adopting Electronic Health Record (EHR) for a patient's record-keeping and Enterprise resource planning (ERP) for enhancing efficiency in internal operations (Chakravorty et al., 2019). Now, in the era of industry 4.0, where all devices are connected seamlessly and integrated. Healthcare sector uses such tools for enhanced flexibility and agility. Sensor empowered IoT enabled wearable health device (WHD) have the enormous potentiality to disrupt healthcare services with data integration and transmission power and opens up a new era of service delivery, which is more flexible, affordable and efficient (Chakraborty & Bhatt, 2019). Wearable devices transmit the physiological data to the provider by cloud services (Rahmani et al., 2015). With integrated and real-time monitoring system provider and other medical professionals can have early intervention and reduces unnecessary patients' visit to the emergency room (Internet Of Healthcare Things In India: Changing The Landscape, n.d.; Riding Technology: The Role of IoT in Healthcare Surveillance - The Economic Times, n.d.; Thompson et al., 2020).
Most of the literature is focused based on the antecedent to the adoption of WHD. The research includes the study of the adoption models like UTAUT 2 (Talukder et al., 2020), TAM (Papa et al., 2020), TRA and TBP (Mital et al., 2018) which measures the antecedents to adopt WHD. However, mainstream literature focuses on efficiency and effectiveness of WHD for health monitoring for chronic as well as acute disease (Godinho et al., 2016; Kekade et al., 2018). However, adoption studies did not study the outcome of adoption like better services, and the other stream of research was able to find out the result. Yet, to the best of the knowledge, no study has been performed, which includes the outcome as a service disruption.
This empirical study focuses on the patients' adoption of wearable devices and establishes a scenario of healthcare service delivery disruption. The study investigates the importance of wearable device adoption and its impact on service engagement as well as collaborative decision making. The study tries to understand and analyze the influence of patient-provider interaction and how wearable device adoption enhances patient-provider communication, collaborative decision making and ultimately leads to service engagement.
Theoretical Framework and Hypotheses Development
Emotional bonding and attachment theory
Humans tend to attach with person and objects which fulfils their need (Hudson et al., 2018). Adults are likely to make an affectionate bond with the family and friends as they provide security and comfort to grow in a better way (Shaver & Mikulincer, 2010). In the same way, a patient feels helpless during illness and may start to experience fatigue, stress or loneliness they tend to make an affectionate bond with the medical care provider, family members and even technology (Li et al., 2020). With its capabilities, WHD offers self- monitoring of physiological symptoms and disrupts the traditional healthcare delivery system. This modern care delivery system empowers patient and makes them responsible for their health (Iverson et al., 2008). WHD adoption enables physicians also to provide universal care (Sodhro et al., 2018) and because of the ubiquitous care patient feels provider is always there to help. This feeling enables emotional bonding towards provider and attachment towards technology.
Service-Dominant Logic (S-D Logic)
Opposed to the goods dominant (G-D) logic based on the push philosophy, service- dominant (S-D) logic theorizes the value creation by intervention and works on the philosophy of 'Value-in-Use' (Lusch & Vargo, 2006; Vargo & Lusch, 2008). Healthcare value is created when the provider interacts with the patient to give relief from pain (Vargo & Lusch, 2008). Thus, value is jointly produced by the provider and the patient. With WHD adoption enabled ubiquitous healthcare delivery system; the provider is empowered to monitor the patient remotely. WHD also empowers provider to intervene early, which leads to early interaction with the patient to avoid dared consequences as for specific disease management becomes easy if identified at an early stage.
Wearable Health Device (WHD) Adoption
WHD is a combined IoT enabled cloud systems which can connect pervasively and interacts in a synchronized habitat defined as 'a system of gadgets, sensors, devices, actuators, hardware, software and programming which creates the interface for the interaction and helps in collaborating, synchronizing and transmitting the vital information with the liked components' (Lom et al., 2016). WHD enables the patient to self-monitor vital symptoms (Fitbit Versa 2 | Health & Fitness Smartwatch, n.d.) and shows a healthy way to live life by sending a regular notification about health status and how to improve it (Samsung Galaxy Watch Active 2 - Specs & Features | Samsung India, n.d.). For chronic as well as acute disease WHD can be useful as it can measure body fat, female health, calorie, heart rate (Deshkar et al., 2017). WHD tracks daily activity and exercise and enables youngsters to stay healthy (Lunney et al., 2016). With its enormous capabilities, WHD transmits real-time data with complete serialization to the provider for decision making based on analytical frameworks (Bhatt et al., 2019) through the cloud-enabled platform (Hassan et al., 2014). The capability of capturing and transmitting the raw signals in real-time enables pervasive computing and provides ubiquitous information (Konstantinidis et al., 2015). Therefore, it can be hypothesized that,
H1: WHD adoption is positively related with the Information Pervasiveness
Information Pervasiveness
Real-time data must be transmitted transparency to the provider and other stakeholders. Physicians can provide sufficient attention as data is readily available to them (Lulembo & Silumbe, 2016). The patient can discuss important things about health and wellbeing during the consultation (online or offline), and the interaction session is not just a question-answer (Q&A) session, which creates value for the healthcare service provider (Osei-Frimpong et al., 2018). WHD adoption also enables time-independent consultation session as every time patients' visit to the provider is not necessary (Plageras et al., 2016). Pervasive information systems enable ubiquitous healthcare delivery, where the provider can give equal attention to the entire patient, and the patient also feels that the provider is just a click away.
H2: Level of information pervasiveness is positively related to the provider-patient interaction.
Information pervasiveness helps provider in decision making during the treatment cycle. On the other side, it also helps in the prevention of medical conditions (Portela et al., 2014). Patient, as well as provider, has access to the same data and patients are empowered to gain knowledge. When the patient can observe their health conditions, they tend to actively participate in the decision-making process as the patient is aware of their health and studies the pros and cons of treatment.
H3: Level of information pervasiveness is positively related to the collaborative decision making
Provider-Patient Interaction
Interaction requires collaborative relationships and mutual trust (Alam, 2013). Cooperation between provider and patient is vital for value creation (Blumstein, 1994). Patient- provider interaction is all about satisfying the patient by identifying the health issue and effectively respond to it (Bove & Johnson, 2000). Although pervasive information obtained by WHD adoption enables the patient to self-monitor medical conditions (Appelboom et al., 2014; Lupton, 2013; Vera-Aguilera et al., 2019), and find related documents over the internet, it is essential that provider also discuss available alternatives, potential threat and outcome of each substitute and values (monetary value) of each (Deber, 1994). Which means that collaborative decision making is not possible without mutual understanding and interaction between provider and patient.
H4: Level of Provider-Patient Interaction is positively related to the level of collaborative decision making.
On the other hand, "service engagement is an extent to which care service is delivered and received between provider and patient with the consideration of all factors influencing patients' experience" (Osei-Frimpong et al., 2018). WHD adoption enables remote consultation and remote interaction between provider and patient. Thus, universal care can be provided, and physicians are in a better position to consult patient, which ameliorates patients' confusion due to the overload of information obtained from WHD as well as internet search. Delivery of healthcare services enhances only when patient satisfaction is achieved by fulfilment of the need for disease management (Polese et al., 2016). Self-monitoring patients tend to feel responsible for their health and tend to improve their approach for care delivery by improving engagement with the provider (Jamal et al., 2015).
H5: Level of Provider-Patient Interaction is positively related to the level of Service Engagement
Collaborative Decision Making
It has been identified that when a patient is empowered enough to take part in the process of decision making along with the provider, it enhances patient trust in treatment and satisfaction (Digital Health Ecosystems: A Payer Perspective | McKinsey, n.d.). With the help of self-monitoring, patients are now more informed about their health and desired to be a part of the decision making process (Osei-Frimpong et al., 2018). An informed patient must be involved in the decision-making process (McColl-Kennedy et al., 2012) as a non-involved patient might not adhere to the treatment protocols and does not shows the engagement (Britten et al., 2000). Involved patients tend to research on their own also for finding the alternatives of treatment and for asking the queries related to wellbeing, which enhances patients' engagement in healthcare service delivery. Service engagement is all about co-creation between patient and provider when a patient is a part of the decision making process better service engagement can be created.
H6: Level of collaborative decision making is positively related to the level of service engagement
Research Methodology
Data Collection
For assessing the proposed relationships, this empirical study uses a survey-based questionnaire, which was sent to the group of WHD users via email. The research involves WHD users and selects the respondents on the criteria that the respondent must have at least six months of experience with WHD. An email along with the cover letter describing the study was sent followed by one reminder after twenty days. Total of 131 usable responses was received, indicating as an accepted sample size in Table 1.
| Table 1 Respondent Demographics | ||
| No. | Percentage | |
| Age | ||
| Less than 25 Years | 28 | 21.4% |
| 25 – 30 Years | 40 | 30.5% |
| 30 – 35 Years | 32 | 24.4% |
| 35 – 40 Years | 20 | 15.3% |
| 40 Years and above | 11 | 8.4% |
| Gender | ||
| Male | 74 | 56.5% |
| Female | 57 | 43.5% |
| Income Level | ||
| Less than 5 LPA | 21 | 16.0% |
| 5 to 10 LPA | 36 | 27.5% |
| 10 to 15 LPA | 41 | 31.3% |
| 15 to 25 LPA | 23 | 17.6% |
| 25 LPA and above | 10 | 7.6% |
Measures
The study includes five different constructs. Developed scales have been used and adapted to the present context of the study. For assessing the initial validity of Q sort methodology (Moore & Benbasat, 1991) was applied with the help of six academicians having publications in a similar area. Inter judge score, items placement ratio and Cohen's kappa value above 0.90 indicated acceptable initial validity of constructs.
With the development of face validity, exploratory factor analysis was conducted with varimax rotation. Table 2 describes items in detail that has been considered in the study.
| Table 2 Construct and Measurement Items | ||
| Construct | Items | Reference |
| Wearable Health Device Adoption | WHDA1- I intend to use wearable health device daily WHDA2- I intend to use wearable health device at every possible opportunity in my day to day life WHDA3- I plan to increase the usage of wearable health device in the future | (Mital et al., 2018; Talukder et al., 2020) |
| Information Pervasiveness | INPV1- Wearable health device updates me regarding events that may affect my health INPV2- It is easy to share health regarding data with the physician from a remote location INPV3- Wearable health device shares notifications to the provider when needed | (Prahalad & Ramaswamy, 2004; Prajogo & Olhager, 2012) |
| Patient-Provider Interaction | PPIN1- provider provided enabling environment for me to actively participate in consultation PPIN2- provider has a good rapport with me PPIN3- Provider discusses vital things which are important to me PPIN4- interaction was more conversational | (Daniel & Darby, 1997; Osei- Frimpong et al., 2018) |
| Collaborative Decision Making | CODM1- Provider asks me to suggest treatment options CODM2- Provider encourages my suggestion on a treatment plan CODM3- Provider discusses the prescription with me CODM4- We together plan for my wellbeing | (Hausman, 2004; Osei- Frimpong et al., 2018) |
| Service Engagement | SREN1- The level of care service provided to me is excellent SREN2- Provider is empathetic to my health condition SREN3- a combined effort by my provider and me is improving the level of care I am receiving | (Salanova et al., 2005) |
Non-response Bias
Non-response bias was examined for assessing the significant difference between the early respondents and slow-wave of responses (Armstrong & Overton, 1977). No significant difference was observed among the two streams of responses: this way suggesting non- existence of any substantial non-response bias.
Common Method Bias
Hermann's single factor test has been used to test common method bias. With the five apparent factors emerged, 38.32 per cent variance explained by the first factor below the benchmark of 50 per cent (Flynn et al., 2010). The factor structure did not show any single factor explaining more than 50 per cent of variance; thereby confirming non-appearance of an only factor and thus satisfying the guideline techniques.
Data Analysis and Findings
Data Analysis
PLS-SEM has been used utilizing using Smart PLS 3.0. As the study aims to evaluate the improvement in healthcare services engagement, use of PLS-SEM has been found the appropriate and logical for the perception-based study (Leguina, 2015). As PLS-SEM is free from the normality assumption, complex models with a smaller sample size efficiently estimated. As a common practice, the PLS-SEM was used to evaluate measurement and structural model.
Measurement Model
In measurement model reliability measured using Cronbach's alpha whereas, validity measured using Average Variance Extracted (AVE) values and item loadings. Value of Cronbach's alpha above 0.7 suggested the internal consistency (Henseler et al., 2009). In contrast, AVE>0.5 (Fornell & Larcker, 1981) and composite reliability>0.7 (Hair et al., 2010) suggested acceptable convergent validity for constructs in Table 3. Acceptable discriminant validity also assessed using Fornell - Larcker criterion (Henseler et al., 2014) as indicated in Table 4.
| Table 3 Item Loading, Composite Reliability, Ave and Cronbach's Alpha | |||||
| Construct | Items Coding | Item Loadings | Composite Reliability | AVE | Cronbach’s Alpha |
| Wearable Health Device Adoption | IoTA1 IoTA2 IoTA3 | 0.698 0.765 0.790 | 0.801 | 0.575 | 0.797 |
| Information Pervasiveness | INPV1 INPV2 INPV3 | 0.841 0.791 0.709 | 0.801 | 0.579 | 0.790 |
| Patient- Provider Interaction | PPIN1 PPIN2 PPIN3 PPIN4 | 0.730 0.839 0.774 0.797 | 0.897 | 0.690 | 0.895 |
| Collaborative Decision Making | CODM1 CODM2 CODM3 CODM4 | 0.771 0.759 0.738 0.778 | 0.871 | 0.633 | 0.867 |
| Service Engagement | SREN1 SREN2 SREN3 | 0.752 0.780 0.826 | 0.807 | 0.593 | 0.789 |
| Table 4 Discriminant Validity–Fornell-Lacker | |||||
| CODM | INPV | PPIN | SREN | WHDA | |
| CODM | 0.796 | ||||
| INPV | 0.593 | 0.761 | |||
| PPIN | 0.682 | 0.554 | 0.830 | ||
| SREN | 0.434 | 0.377 | 0.509 | 0.770 | |
| WHDA | 0.596 | 0.535 | 0.62 | 0.637 | 0.758 |
Structural Model
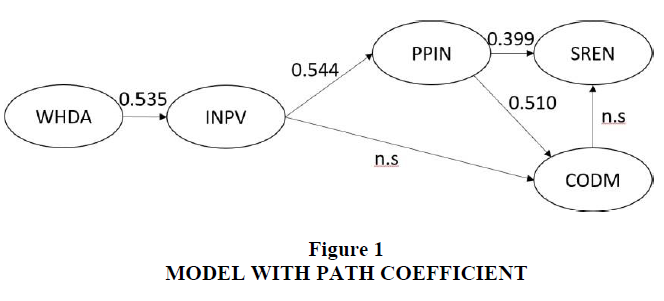
The structural model assessed with bootstrapping using 1000 subsamples (Li et al., 2020) which tested the relationship by path coefficient and t-statistics. As shown in Figure 1, four hypotheses are significant at 1% level of significance, whereas two hypotheses found to be insignificant. As we hypothesized, results revelled significance importance of WHD Adoption on information pervasiveness. It also revealed that Provider-Patient interaction has a significant positive impact on collaborative decision making and service engagement. However, no direct relationship has been established significantly between Information Pervasiveness and Collaborative decision making and Collaborative decision making to service engagement.
Discussion
Unlike other studies on IoT wearables and WHD (Mital et al., 2018; Papa et al., 2020; Talukder et al., 2020) present study concentrates on the consequences of WHD adoption and provide deep imputes to understand and validate how service engagement can be improved with WHD adoption. Wearable Health Device Adoption has a significant positive impact on information pervasiveness. WHDA, which highlights the user's intention to use wearable health device daily, for all possible opportunity instances of the day and also which attempts at capturing whether the user wants to increase its usage in the future, indicate and highlight the enormous amount of related data being gathered through those devices which foster availability of data of all instances that may affect patient health and seamlessly connecting and sharing with the physician from a remote location, facilitating superior care delivery and care-oriented diagnosis, besides giving alarm notification on the go regarding specific health inputs to the provider, enabling an informed care decision environment. As per the rationale and also as expected from the existing literature, the pervasiveness of information positively and significantly impacts patient-provider interaction. Pervasive information environment enables the patient to actively participate in a consultation with the physician; facilitating the development of a good rapport between the patient and physicians, which in turn helps discuss many trivial yet vital things which are instrumental for superior patient care planning and delivery of quality care. This available information pervasiveness creates a platform for high- frequency interactions which are more conversational.
Information pervasiveness has a positive impact on collaborative decision making. With the available plethora of information, the provider gets enough information to plan alternative approaches to patient treatment. Information pervasiveness gives the patient-provider with all possible support and treatment alternative regarding various available treatment options, which comes very handy and as encouragement regarding treatment plans. With all available information and knowledge of other options, the provider can discuss the prescription with the patients and primary patient care providing attender; thereby enabling a constructive planning environment aimed at patient wellbeing. So information pervasiveness and patient-provider interaction create the platform conducive for collaboratively deciding on treatment plans and alternatives.
Further in this study, the empirical investigation highlights that patient-provider interaction and collaborative decision making, both together and individually have positive impacts on the concept of service engagement which is pivotal for any service-centric environment in creating a pleasant and enjoyable service encounter experience. Service engagement which in the current context, encompasses the level of care service provided to the patient in an empathetic way aimed at improving the standard of care experience received for the patient or principle caregiver for the patient. Thus the nuanced underlying nexus helps build a synergistic understanding regarding the antecedent consequent linkages towards care service engagement and experience for patients.
Implications
The study empirically examines the micro-level interaction process between provider- patient dyad. It describes how WHD adoption enhances data availability and help provider to improve patient engagement in healthcare services. The finding supports the theory of S-D logic (Lusch & Vargo, 2006; Vargo & Lusch, 2008) in the context of WHD adoption and service engagement. The study reveals the understanding that it is the interaction between provider and patient, which empowers the patient to take part in the collaborative decision making. The research empirically shows the importance of technology adoption in healthcare service management and states that WHD adoption enhances patients' engagement and interest in the healthcare process. This finding is in line with (Iverson et al., 2008). The investigation adds the consequent of WHD adoption in healthcare service delivery context, from the patients' point of view, which was not studied by eminent scholars.
The study develops a rich understanding of the robustness of technology with the help of a construct 'Pervasiveness'. Patient, as well as provider, adopts WHD when it provides secure access and data policy is robust, which complies with the national law. A developer can look for big data-enabled cloud-based data retrieval system by which personalized care can be provided (Bhatt & Chakraborty, 2020). The investigation also helps the healthcare administrators to understand the changing scenario of care service delivery and patients' readiness to adopt novel technology. The provider may think about providing patient-oriented and patient-centric healthcare involving the patient into the decision making process.
Limitation and Future Scope
The current empirical study is experiencing the issue of generalizability like any other study. On the other hand, the study collected data in a cross-sectional manner, where the learning curve of the user is not captured. However, it is possible that with spending more time user becomes equipped for utilizing such innovatively propelled gadgets, and self-efficacy can be improved. Time-series study has not been conducted to capture the improved user engagement into healthcare service delivery process. However, significant importance was given to the non-
response bias and standard method bias. In the future, the investigation can be done by incorporating the time series model.
Conclusion
The study empirically established a relationship between WHD adoption and care service engagement with theoretical support from emotional bonding and attachment theory as well as service-dominant logic. While attachment theory helps to explain the need of the patient to use WHD and service-dominant logic describes why it is essential for the provider to empower patient for collaborative decision making as well as enhancing patients' engagement in care service delivery process. The investigation enlightens the viewpoint of 'value – in - use' using the partial least square structural equation modelling (PLS-SEM) model with 1% significance level which provides methodological rigour and concludes that WHD adoption enhances patients engagement in care service delivery process and empowers the patient to make collaborative decision making by understanding the disease and treatment option in depth during the interaction with a physician. With a specific limitation of generalizability and adoption curve, the study provides useful information and implications in academic as well as in industry perspective to the provider, administrators and WHD developers to understand the post-adoption behaviour of the patient.
References
- Alam, I. (2013). Customer interaction in service innovation: evidence from India. International Journal of Emerging Markets.
- Appelboom, G., Camacho, E., Abraham, M.E., Bruce, S.S., Dumont, E.L.P., Zacharia, B.E., D’Amico, R., Slomian, J., Reginster, J.Y., Bruyère, O., & Connolly, E.S. (2014). Smart wearable body sensors for patient self-assessment and monitoring. In Archives of Public Health.
- Armstrong, J.S., & Overton, T.S. (1977). Estimating Nonresponse Bias in Mail Surveys. Journal of Marketing Research.
- Bhatt, V., & Chakraborty, S. (2020). Implications of IT Infrastructure and Big Data Characteristics on SCOR Model for Performance Measurement. International Journal of Recent Technology and Engineering, 8(5), 1748–1756. https://doi.org/10.35940/ijrte.e6300.018520
- Bhatt, V., Sashikala, P., & Chakraborty, S. (2019). The impact of information technology and analytics on the performance of a hospital: Scale development in Indian context. International Journal of Recent Technology and Engineering, 8(3), 2861–2869. https://doi.org/10.35940/ijrte.C5229.098319
- Blumstein, J.F. (1994). Health care reform and competing visions of medical care: antitrust and state provider cooperation legislation. Cornell Law Review.
- Bove, L.L., & Johnson, L.W. (2000). A customer-service worker relationship model. International Journal of Service Industry Management.
- Britten, N., Stevenson, F.A., Barry, C.A., Barber, N., & Bradley, C.P. (2000). Misunderstandings in prescribing decisions in general practice: Qualitative study. British Medical Journal.
- Chakraborty, S., & Bhatt, V. (2019). Mobile IoT adoption as antecedent to Care-Service Efficiency and Improvement: Empirical study in Healthcare-context. Journal of International Technology and Information Management, 28(3), 101–120.
- Chakravorty, T., Jha, K., & Barthwal, S. (2019). Linking EHR and ERP adoption with flexibility in care-delivery and operational performance: A conceptual review in hospital supply chain. Indian Journal of Public Health Research and Development. https://doi.org/10.5958/0976-5506.2019.01247.6
- Daniel, K., & Darby, D.N. (1997). A dual perspective of customer orientation: A modification, extension and application of the SOCO scale. International Journal of Service Industry Management. https://doi.org/10.1108/09564239710166254
- Deber, R.B. (1994). Physicians in health care management: 8. The patient-physician partnership: Decision making, problem solving and the desire to participate. In CMAJ.
- Deshkar, S., A, T.R., & Menon, V.G. (2017). A review on IoT based m-Health systems for diabetes. In International Journal of Computer Science and Telecommunications (Vol. 8, Issue 1). www.ijcst.org
- Fitbit Versa 2 | Health & Fitness Smartwatch. (n.d.). Retrieved April 19, 2020, from https://www.fitbit.com/in/versa
- Flynn, B.B., Huo, B., & Zhao, X. (2010). The impact of supply chain integration on performance: A contingency and configuration approach. Journal of Operations Management. https://doi.org/10.1016/j.jom.2009.06.001
- Fornell, C., & Larcker, D. F. (1981). Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. Journal of Marketing Research, 18(1), 39–50. https://doi.org/10.2307/3151312
- Godinho, C., Domingos, J., Cunha, G., Santos, A. T., Fernandes, R. M., Abreu, D., Gonçalves, N., Matthews, H., Isaacs, T., Duffen, J., Al-Jawad, A., Larsen, F., Serrano, A., Weber, P., Thoms, A., Sollinger, S., Graessner, H., Maetzler, W., & Ferreira, J. J. (2016). A systematic review of the characteristics and validity of monitoring technologies to assess Parkinson’s disease. In Journal of NeuroEngineering and Rehabilitation.
- Hair, J.F., Black, W.C., Babin, B. J., & Anderson, R.E. (2010). Multivariate Data Analysis. In Vectors.
- Hassan, M. M., Albakr, H. S., & Al-Dossari, H. (2014). A cloud-assisted Internet of Things framework for pervasive healthcare in smart city environment. EMASC 2014 - Proceedings of the 1st International Workshop on Emerging Multimedia Applications and Services for Smart Cities, Workshop of MM 2014, 9–13. https://doi.org/10.1145/2661704.2661707
- Hausman, A. (2004). Modeling the patient-physician service encounter: Improving patient outcomes. Journal of the Academy of Marketing Science. https://doi.org/10.1177/0092070304265627
- Henseler, J., Ringle, C.M., & Sarstedt, M. (2014). A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science. https://doi.org/10.1007/s11747-014-0403-8
- Henseler, J., Ringle, C.M., & Sinkovics, R.R. (2009). The use of partial least squares path modeling in international marketing. Advances in International Marketing. https://doi.org/10.1108/S1474-7979(2009)0000020014
- Hudson, D., Kushniruk, A., Borycki, E., & Zuege, D.J. (2018). Physician satisfaction with a critical care clinical information system using a multimethod evaluation of usability. International Journal of Medical Informatics, 112, 131–136.
- Iverson, S.A., Howard, K.B., & Penney, B.K. (2008). Iverson et al • Special Communication Impact of Internet Use on Health-Related Behaviors and the Patient- Physician Relationship: A Survey-Based Study and Review. In J Am Osteopath Assoc (Vol. 108). http://jaoa.org/
- Jamal, A., Khan, S.A., AlHumud, A., Al-Duhyyim, A., Alrashed, M., Shabr, F. Bin, Alteraif, A., Almuziri, A., Househ, M., & Qureshi, R. (2015). Association of online health information - Seeking behavior and self-care activities among type 2 diabetic patients in Saudi Arabia. Journal of Medical Internet Research, 17(8), 1–15. https://doi.org/10.2196/jmir.4312
- Kekade, S., Hseieh, C.H., Islam, M.M., Atique, S., Mohammed Khalfan, A., Li, Y.C., & Abdul, S.S. (2018). The usefulness and actual use of wearable devices among the elderly population. Computer Methods and Programs in Biomedicine, 153(1), 137–159. https://doi.org/10.1016/j.cmpb.2017.10.008
- Konstantinidis, E.I., Sidiropoulos, E.A., Conci, N., De Natale, F., Bamparopoulos, G., & Bamidis, P.D. (2015). Introducing Neuroberry, a platform for pervasive EEG signaling in the IoT domain. MOBIHEALTH 2015 - 5th EAI International Conference on Wireless Mobile Communication and Healthcare - Transforming Healthcare through Innovations in Mobile and Wireless Technologies. https://doi.org/10.4108/eai.14-10-2015.2261698
- Leguina, A. (2015). A primer on partial least squares structural equation modeling (PLS- SEM). International Journal of Research & Method in Education. https://doi.org/10.1080/1743727x.2015.1005806
- Li, J., Zhang, C., Li, X., & Zhang, C. (2020). Patients’ emotional bonding with MHealth apps: An attachment perspective on patients’ use of MHealth applications. International Journal of Information Management, 51(December), 102054. https://doi.org/10.1016/j.ijinfomgt.2019.102054
- Lom, M., Pribyl, O., & Svitek, M. (2016). Industry 4.0 as a part of smart cities. 2016 Smart Cities Symposium Prague, SCSP 2016. https://doi.org/10.1109/SCSP.2016.7501015
- Lulembo, O.M., & Silumbe, R. (2016). Improving healthcare delivery with the use of online patient information management system. 2016 IST-Africa Conference, IST-Africa 2016. https://doi.org/10.1109/ISTAFRICA.2016.7530679
- Lunney, A., Cunningham, N.R., & Eastin, M.S. (2016). Wearable fitness technology: A structural investigation into acceptance and perceived fitness outcomes. Computers in Human Behavior. https://doi.org/10.1016/j.chb.2016.08.007
- Lupton, D. (2013). The digitally engaged patient: Self-monitoring and self-care in the digital health era. Social Theory and Health. https://doi.org/10.1057/sth.2013.10
- Lusch, R.F., & Vargo, S.L. (2006). Service-dominant logic: Reactions, reflections and refinements. Marketing Theory, 6(3), 281–288. https://doi.org/10.1177/1470593106066781
- McColl-Kennedy, J.R., Vargo, S.L., Dagger, T.S., Sweeney, J.C., & van Kasteren, Y. (2012). Health Care Customer Value Cocreation Practice Styles. Journal of Service Research, 15(4), 370–389. https://doi.org/10.1177/1094670512442806
- McKinsey. Digital health ecosystems: A payer perspective | (n.d.). Retrieved April 22, 2020, from https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/digital-health-ecosystems-a-payer-perspective
- Mital, M., Chang, V., Choudhary, P., Papa, A., & Pani, A. K. (2018). Adoption of Internet of Things in India: A test of competing models using a structured equation modeling approach. Technological Forecasting and Social Change, 136, 339–346. https://doi.org/10.1016/j.techfore.2017.03.001
- Moore, G.C., & Benbasat, I. (1991). Development of an instrument to measure the perceptions of adopting an information technology innovation. Information Systems Research. https://doi.org/10.1287/isre.2.3.192
- Optum Internet Of Healthcare Things In India: Changing The Landscape. (n.d.). Retrieved April 17, 2020, from http://www.optum.in/thought-leadership/library/internet-healthcare- things.html
- Osei-Frimpong, K., Wilson, A., & Lemke, F. (2018). Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technological Forecasting and Social Change, 126, 14–27. https://doi.org/10.1016/j.techfore.2016.04.009
- Papa, A., Mital, M., Pisano, P., & Del Giudice, M. (2020). E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technological Forecasting and Social Change. https://doi.org/10.1016/j.techfore.2018.02.018
- Plageras, A.P., Psannis, K.E., Ishibashi, Y., & Kim, B.G. (2016). IoT-based surveillance system for ubiquitous healthcare. IECON Proceedings (Industrial Electronics Conference). https://doi.org/10.1109/IECON .2016.7793281
- Polese, F., Tartaglione, A.M., & Cavacece, Y. (2016). Patient empowerment for healthcare service quality improvements: a value co-creation view. In 19th Toulon-Verona International Conference: Excellence in Services (pp. 385–398).
- Portela, F., Santos, M.F., MacHado, J., Abelha, A., Silva, Á., & Rua, F. (2014). Pervasive and intelligent decision support in intensive medicine - The complete picture. Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). https://doi.org/10.1007/978-3-319-10265-8_9
- Prahalad, C.K., & Ramaswamy, V. (2004). Co-creation experiences: The next practice in value creation. Journal of Interactive Marketing. https://doi.org/10.1002/dir.20015
- Prajogo, D., & Olhager, J. (2012). Supply chain integration and performance: The effects of long-term relationships, information technology and sharing, and logistics integration. International Journal of Production Economics. https://doi.org/10.1016/j.ijpe.2011.09.001
- Rahmani, A.M., Thanigaivelan, N K., Gia, T.N., Granados, J., Negash, B., Liljeberg, P., & Tenhunen, H. (2015). Smart e-Health Gateway: Bringing intelligence to Internet-of- Things based ubiquitous healthcare systems. 2015 12th Annual IEEE Consumer Communications and Networking Conference, CCNC 2015, July, 826–834. https://doi.org/10.1109/CCNC.2015.7158084
- Salanova, M., Agut, S., & Peiró, J.M. (2005). Linking organizational resources and work engagement to employee performance and customer loyalty: The mediation of service climate. In Journal of Applied Psychology. https://doi.org/10.1037/0021-9010.90.6.1217
- Samsung India - Samsung Galaxy Watch Active 2 Specs & Features | (n.d.). Retrieved April 19, 2020, from https://www.samsung.com/in/microsite/galaxy-watch-active2/
- Shaver, P.R., & Mikulincer, M. (2010). New directions in attachment theory and research. Journal of Social and Personal Relationships, 27(2), 163–172. https://doi.org/10.1177/0265407509360899
- SmartPLS, Discriminant Validity Assessment |. (n.d.). Retrieved April 30, 2020, from https://www.smartpls.com/documentation/algorithms-and-techniques/discriminant- validity-assessment
- Sodhro, A.H., Sangaiah, A.K., Sodhro, G.H., Lohano, S., & Pirbhulal, S. (2018). An energy-efficient algorithm for wearable electrocardiogram signal processing in ubiquitous healthcare applications. Sensors (Switzerland). https://doi.org/10.3390/s18030923
- Talukder, M.S., Sorwar, G., Bao, Y., Ahmed, J.U., & Palash, M.A.S. (2020). Predicting antecedents of wearable healthcare technology acceptance by elderly: A combined SEM-Neural Network approach. Technological Forecasting and Social Change, 150(June 2019), 119793. https://doi.org/10.1016/j.techfore.2019.119793
- The Economic Time, Riding technology: The role of IoT in healthcare surveillance (n.d.).Retrieved April 17, 2020, from https://m.economictimes.com/small-biz/security- tech/technology/riding-technology-the-role-of-iot-in-healthcare- surveillance/articleshow/59710658.cms
- Thompson, S., Whitaker, J., Kohli, R., & Jones, C. (2020). Chronic Disease Management: How IT and Analytics Create Healthcare Value Through the Temporal Displacement of Care. MIS Quarterly, 44(1), 227–256. https://doi.org/10.25300/misq/2020/15085
- Vargo, S.L., & Lusch, R.F. (2008). Service-dominant logic: Continuing the evolution. Journal of the Academy of Marketing Science, 36(1), 1–10.
- Vera-Aguilera, J., Haji-Abolhassani, I., Kulig, K., Heitz, R., Paludo, J., Ghoreyshi, A., Scheevel, J. R., Schimke, J. M., & Markovic, S. N. (2019). Early Fever Detection By a Novel Wearable Continuous Temperature Monitor in Patients Undergoing Autologous Stem Cell Transplantation. Blood. https://doi.org/10.1182/blood-2019-125159