Research Article: 2025 Vol: 29 Issue: 5
Leveraging Artificial Intelligence for Sustainable Healthcare Marketing: Opportunities and Ethical Challenges
Sunday Clement, DBA Student, Rushford Business School, Rushford, Switzerland
Citation Information: Clement, S. (2025). “Leveraging artificial intelligence for sustainable healthcare marketing: opportunities and ethical challenges". Academy of Marketing Studies Journal, 29(5), 1-9.
Abstract
This paper will explore the evolving role of Artificial Intelligence (AI) in healthcare, highlighting its transformative impact on diagnostics, treatment personalization, operational efficiency, and patient engagement. It discusses the role of AI in sustainable healthcare systems in terms of sustainable use of resources and ecological, economic and social goals related to the United Nations Sustainable Development Goals (SDGs). The research also raises ethical concerns about adopting AI, such as bias, transparency, privacy, and the importance of human oversight to ensure fair and responsible usage. It also examines new regulatory landscapes, including the European AI Act and the European Health Data Space, which were formed to facilitate AI's safe and ethical deployment in healthcare. The findings emphasize that while AI holds great promise to revolutionize healthcare delivery, careful governance and multidisciplinary collaboration are essential to maximize benefits and mitigate risks. This paper advocates for a balanced, patient-centred approach integrating innovation with ethical and sustainability commitments to create more intelligent, inclusive healthcare systems.
Keywords
Artificial Intelligence, Healthcare, Sustainability, Ethical AI, Patient Engagement, Sustainable Development Goals, AI Regulation, Healthcare Innovation.
Introduction
There is growing pressure on healthcare organizations worldwide to meet the 'quadruple aim'- to improve the population's health, enhance patient care experience, improve the providers' work life, and reduce care costs. Ageing populations, an increasing burden of chronic diseases and unsustainable healthcare expenses are compelling governments, payers, regulators and providers to redesign and innovate around new models of care. The COVID-19 pandemic has heightened calls for such demands (e.g. staff shortages and equity of access), which have revealed failures in systems, which have long since been pointed out by World Health Organization (Bhatia et al. 2023).
In reaction, an increasing focus is being placed on using data in the real world to execute and, more broadly, 'transform' healthcare at scale. The integration of Artificial Intelligence (AI) into healthcare systems has emerged as a pivotal solution to address these dual imperatives. The convergence of technological advancements—including cloud computing, the Internet of Things (IoT), enhanced computing power, and robust data security frameworks with increasingly available multimodal data (such as genomics, demographic, clinical, and behavioral data) is setting the stage for a significant evolution in AI-augmented healthcare (Thomas, 2024).
Even with high standards of care, many hospitals and healthcare systems have already begun to mitigate their environmental footprint on patients, staff and the surrounding community. An increasing body of evidence has found that addressing sustainability in healthcare settings—from waste and infrastructure to safer chemicals and cost savings—has also translated into improved environmental performance, patient satisfaction, employee health and well-being, and community-wide health. These initiatives also cover new areas like care-from-a-distance and accessibility of healthcare in rural accessible sores, which reflect the industry’s increasing commitment to equitable and sustainable delivery of care (Bhatia, et al. 2023). Meanwhile, artificial intelligence radically changes how healthcare is delivered, impacting prevention, diagnosis, and treatment and patient services. AI has the potential to help ease physician workloads, improve availability, and improve responses to health emergencies.
However, in healthcare sector the effectiveness of AI is determined by not only the technical side of it such as reliability, accuracy and usability, but also the human aspect such as trust, acceptability and adaptability. With new AI-powered breakthroughs, the solutions can disrupt existing workflows with potential resistance or anxiety from medical professionals. Hence, it is vital to recognize the duality of implications of the technology, i.e., the technology not only brings the possibility of improvement in environmental sustainability and technological advancement but also results in human-centric adoption (Bajwa et al. 2021). Thus, understanding this interplay between technology and behaviour is crucial for AI's responsible and effective integration in healthcare markets and delivery (Bajwa et al. 2021).
AI is increasingly embedded throughout marketing stacks, enabling end-to-end, omnichannel strategies that result in more efficiency, personalization and reach. As the reliance on AI automation becomes even more essential, it has become crucial for marketing and regulators to ensure AI is intended and used responsibly, ethically, and transparently. In this journal article, the potential impact of AI on sustainable healthcare marketing is explored, with critical reflection on ethical considerations and governance structures that should guide its use.
Research Methodology
This research uses a qualitative exploratory design to investigate the possibilities and ethical issues of applying artificial intelligence (AI) to sustainable healthcare marketing. With this topic's burgeoning and multi-disciplinary nature, a model-based study allows for the meaningful study of such intervention, along with stakeholder views, regulations and best practices as they develop over time. A semi-structured interview approach is adopted, and interviews with healthcare marketing professionals, AI specialists, and policy analysts will be complemented with secondary analysis of policy position texts, including key documents such as the European AI Act and the European Health Data Space (EHDS). A purposive sampling approach is adopted to recruit participants from different sectors and regions with expertise in the subject matter.
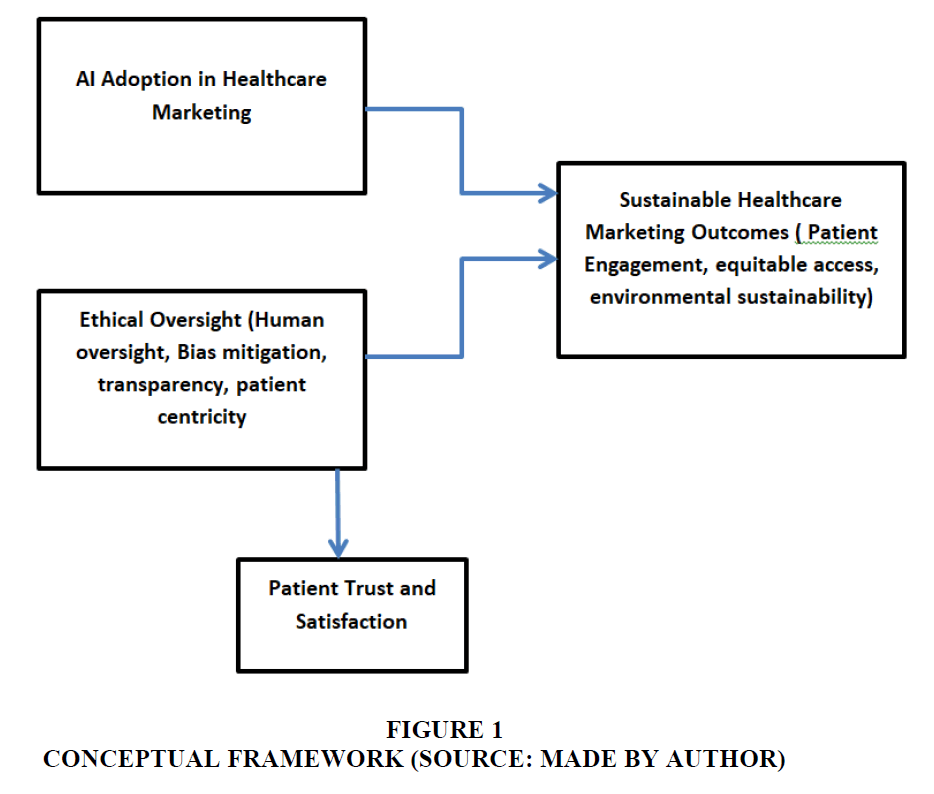
A constructivist paradigm underpins this research, emphasizing the co-construction of meaning through the experiences and perspectives of key stakeholders. The qualitative approach enables a deeper understanding of subjective experiences, institutional practices, and policy implications related to AI adoption in healthcare marketing. Data is analyzed using thematic analysis, guided by a conceptual framework, to identify patterns related to ethical oversight, transparency, bias mitigation, and patient-centric communication. This methodology aligns with the study's conceptual framework, which connects AI integration with sustainable marketing principles and ethical imperatives in healthcare.
Conceptual Framework
The paper is based on an enhanced conceptual framework that connects artificial intelligence (AI) use in healthcare marketing with sustainability outcomes through the moderation of ethics. The framework underscores how operational efficiency, personalization, and patient engagement can be reinforced by AI-based tools and flags ethical risks, such as bias, lack of transparency, and data privacy concerns. By adding in regulatory and human oversight, such as the EU AI Act and EHDS, the model promotes a middle course that promotes sustainable marketing in healthcare. The framework provides basis for analyzing opportunities and challenges in the responsible use of AI Figure 1.
Literature Review
AI in Healthcare: Evolution and Applications
There have been remarkable strides in Artificial Intelligence (AI) in healthcare, from early pioneering expert systems in the 1970s to cutting-edge AI and deep learning models that can support real-time clinical decision-making. Early systems such as MYCIN were forced to factor in computational capacity and data limits (Bajwa et al., 2021c). Moreover, AI is a fundamental part of contemporary healthcare provision with the evolution of big data, cloud infrastructure, and computational algorithms.
AI is being used in multiple industries, including diagnostics, treatment planning and patient engagement. In medical imaging, AI systems have achieved diagnostic sensitivity of over 94% for detecting breast cancer. Notably, AI has significantly reduced false-positive rates by 37.3% and biopsy requests by 27.8% while maintaining high diagnostic sensitivity (Ahn et al., 2023). AI assists healthcare providers in oncology and precision medicine by combining multidimensional datasets to deliver personalized, evidence-based treatment plans.
Meanwhile, AI-powered virtual assistants and chatbots are also changing the game in patient engagement aiding with symptom checking, appointment booking, medication adherence and management of chronic disease. These utilities are associated with a 20% reduction in avoidable visits to the emergency room and an increase of up to 35% in the level of compliance with medication.
Operationally, AI is enhancing efficiency and expanding access to care. Automation of routine administrative tasks such as billing, transcription, and documentation has helped reduce clinician workload by up to 17%, freeing more time for patient care. Economically, AI-driven interventions are projected to save the U.S. healthcare system up to $150 billion annually by 2026 through improved diagnostics, workflow optimization, and preventive care strategies. Importantly, AI is also helping bridge the urban-rural healthcare gap. For example, AI-enabled smartphone-based retinal imaging tools are being deployed in underserved areas to detect conditions like diabetic retinopathy, offering early diagnosis without requiring specialist access (Ahn et al., 2023).
Collectively, the evolution and integration of AI into healthcare systems are enhancing clinical accuracy, operational efficiency, and service accessibility, laying the groundwork for a more intelligent, sustainable, and inclusive healthcare future.
Sustainability in Healthcare Systems
Greening health is a term used to describe the attainment of high-quality care within health sectors that minimizes adverse environmental impacts, ensures economic sustainability and contributes to social equity. This includes environmental sustainability, meaning the reduction of waste, emissions, and resource use; economic sustainability, which looks at cost-efficiency and effectiveness over time; and social sustainability, which is about fair access, worker wellbeing and community involvement. A sustainable health system provides for the needs of the current population while not weakening the capacity of future generations to provide for their needs (Sajwani, 2024).
In practice, healthcare institutions are implementing various sustainable efforts to minimize their environmental impact and enhance system performance. This encompasses environmentally friendly building design, energy efficiency, environmentally sound waste treatment and disposal, and limiting the use of hazardous materials. From the economic standpoint, organizations rationalize procurement, minimize the supply chain, and introduce a preventive care-based model to reduce future costs. Moreover, socially, promoting employees’ safety at work, increasing access to care in underserved communities, or allowing all-inclusive approaches to patient engagement lead to a more equitable system. Hospitals, for example, are incorporating telehealth, electronic records, and community-based care programs in their broader sustainability programs (Bajwa et al., 2021) .
Technology plays a vital part in improving healthcare sustainability. Remote health services, forecasted diagnosis and intelligent health planning, have become real thanks to digital tools and AI-based systems. Telemedicine cuts down on patient travel and physical infrastructure, which reduces emissions. AI and analytics automate workflows, forecast disease outbreaks, and lower unnecessary interventions, while saving money and resources (Sajwani, 2024). Additionally, digital platforms support environmental monitoring and compliance reporting, helping healthcare organizations align with regulatory and sustainability goals.
AI in Healthcare to Achieve the Sustainable Development Goals (SDGs)
Artificial Intelligence (AI) has been a game-changer in pursuing the United Nations’ 2030 Agenda for Sustainable Development. The research found that AI supports 134 of 169 (nearly 79%) SDG targets with improved data analysis, decision processes and service provision (Vinuesa et al., 2020). However, this “potentially harms 35% of targets” if not managed carefully, with concerns around bias, privacy, and inequality (Vinuesa et al., 2020).
Despite only one of the SDGs (Goal 3) being directly related to health, many other SDGs interrelate with it through health. Consequently, the HHSDGs require a unified approach. The attainment of SDG 3 and its corresponding targets requires a cross-sectoral approach to policy and policy coherence across all sectors impacting human health and well-being (Ammi et al., 2024).
To address this, the World Health Organization (WHO) developed a comprehensive list of 100 HHSDG core indicators to serve as a reference for tracking advancement. Based on that, nine priorities have been suggested for national health-responsive planning and implementation of health-related SDGs. These are political and financial commitment, institutional preparedness, stakeholder participation, development partner involvement, multispectral collaboration, equity promotion, capacity development and strong monitoring and evaluation mechanism (SEARO, 2017).
To achieve the most significant impact, governments must integrate SDG targets into national development plans and capitalize on multi-agency governance, policy, and technical expertise. Equity is also really taking on more attention, making sure that vulnerable and underprivileged communities have access to affordable and good-quality care. By strategically integrating AI into these domains, countries can accelerate progress toward achieving universal health coverage and other critical health outcomes in line with the SDG framework.
Ethical Considerations in AI Adoption
As AI continues transforming the healthcare industry, particularly in how organizations approach patient communication and marketing, ethical considerations are becoming increasingly central. AI has the enormous potential to help change the game for healthcare marketers, enhancing personalization, efficiency, engagement, and more. However, the power of AI must be balanced with responsible governance. Without ethical underpinning, its adoption may inadvertently entrench health inequities, erode patient trust, and bring significant concerns concerning data privacy and environmental sustainability (Egert, 2024).
Human oversight is one of the most essential underpinnings of moral AI use. AI models are extremely powerful at data processing and pattern recognition, but they lack the contextual judgment, empathy, and ethical reasoning necessary to support a medical decision. Hence, it is critical to blend skilled human professionals into AI-enabled workflows.
For example, when AI algorithms are used to recommend medical treatments or personalize marketing content, healthcare experts must be involved in interpreting outputs responsibly. Thus, human-AI collaboration allows medical marketing campaigns to retain the human touch and keep it patient-centred and within the lines of healthcare legality and ethical framework. Through continued human oversight, health systems can promote transparent and accountable AI-assisted practices trusted by the public (Egert, 2024).
However, another key issue is the bias underlying AI systems. AI learns from data, and if that data is partial, biased or carries historical bias, the outcomes can reinforce inequality. One illustrative example we have recorded took place in American hospitals, where an artificial intelligence (AI) predictor of patient needs underestimated Black patients' health needs by an average of almost 50% due to inbuilt discriminatory skew. In healthcare marketing, similar risks arise when AI tools personalize content or segment audiences based on flawed assumptions, potentially excluding marginalized communities or disseminating misleading information (Sajwani, 2024). Organizations must conduct regular bias audits to mitigate such issues, utilize diverse and representative data sets, and prioritize inclusive design. Ethical AI cannot be built on biased foundations.
Transparency is the key in ethical use of AI. Patients and healthcare providers have the right to know if and how AI is involved in communications, including content creation. When, for instance, AI-generated videos explain a medical process or a medicine, the stakeholders absolutely must know the degree to which AI has participated. A Deloitte investigation in 2023 discovered that more than 60% of health workers pointed to a lack of transparency as one of the significant obstacles to AI uptake (Egert, 2024). By voluntarily sharing that AI is informing a decision or content generation, it helps industries build credibility and catch up to increased regulatory expectations around explainability and informed consent.
Ideally, patients should remain central to any AI-centered communication strategies. Moreover, although behavioural insights and predictive analytics can significantly improve personalization, healthcare organizations must ensure these tools are deployed to educate and engage patients, not to play them. Ethical advertising should reinforce the patient's autonomy by offering data enabling informed choice rather than nudging toward desired commercial ends. An ethical approach to AI is transparent and fair and supports the patient's right to choose so that marketing remains consistent with wider healthcare ethics. (Bajwa et al., 2021)
In addition to social and regulatory issues, the adoption of AI has environmental consequences. Efficient AI models and training could significantly reduce energy use and carbon emissions. This raises a broader sustainability challenge: How can healthcare marketers leverage AI responsibly without compromising environmental goals? The answer lies in strategic deployment using AI where it has the greatest benefit, optimizing its efficiency, and aligning AI use with an organization's climate and sustainability commitments.
In order to guide through this labyrinth, the European Union has developed a few core policy frameworks. The European Artificial Intelligence Act (AI Act) is a key regulatory proposal that entered into force on 1 August 2024 and aims to promote AI's ethical and safe use within the European Union. Under this legislation, high-risk AI systems must adhere to rigorous standards, including many used in medical devices, diagnostics, and healthcare marketing (Eiropean Commision, 2025). These are strong risk mitigation measures, such as using high-quality and representative training data, human-in-the-loop, and thorough documentation. It also applies to general-purpose AI (GPAI) models, calling for more transparency and creating a specific European AI Office to ensure enforcement. A Code of Practice, expected by April 2025, will guide AI providers and developers on remaining compliant while promoting innovation (Egert, 2024).
Meanwhile, the European Health Data Space (EHDS), which entered into force in 2025, provides another crucial element in the AI ethical puzzle. The EHDS provides safe and fair access to a wide variety of health data for both primary use (in clinical practice) and secondary use (e.g., AI training and research) (Egert, 2024). The EHDS facilitates structured access for analysis to various anonymized data sources so the AI solutions particularly in the health sector have become more trustworthy, accurate and free of bias. Importantly, the EHDS is designed with strong privacy protections, aligning with the General Data Protection Regulation (GDPR), the Data Governance Act, and the Data Act. It fosters innovation while maintaining strict ethical safeguards, ensuring data usage respects individual rights and promoting inclusive AI development (Egert, 2024).
The AI Act, combined with the EHDS, marks a significant step in developing a responsible and ethical AI ecosystem in healthcare. Such regulatory frameworks give companies standards and tools for creating and using AI in a transparent, fair, sustainable, and patient-centric way. By signing up for these, healthcare marketers can embrace AI on a sure footing and ensure their ethics and social responsibility are intact(Eiropean Commision, 2025). The future of healthcare marketing is here and now in smart marketing automation and how well it is used.
The increasing adoption of artificial intelligence (AI) technologies in the healthcare sector has introduced a broad spectrum of new opportunities (Lee & Yoon, 2021). As highlighted by Safavi and Kalis (2019), it is imperative to critically examine AI’s role, particularly by assessing both the potential benefits and the challenges associated with its implementation in healthcare settings.
AI-driven solutions have demonstrated significant potential to improve patient care services, especially in rural and agricultural communities within developing nations (Guo & Li, 2018). These technologies enhance diagnostic accuracy and reduce errors, thereby supporting the delivery of high-quality healthcare at reduced costs. According to ABI Research, the integration of advanced AI applications in the healthcare industry was projected to generate savings of up to $52 billion in the United States by 2021 (AI to Save Healthcare Sector US$52 Billion in 2021) (Zacharakis et al., 2022). As a result, AI-based technologies can potentially transform healthcare delivery by streamlining operations and deepening relationships with clients and patients, thereby creating a more effective and efficient healthcare system.
Despite its transformational promise, artificial intelligence (AI) is not a panacea. As Amann et al. (2020) contend, technological developments have historically introduced new obstacles and complexities. Lee and Yoon (2021) also stress that although AI applications provide creative ways to improve day-to-day living, they also provide barriers that need to be overcome. This needs a multidisciplinary approach, as some issues are technical, while others are legal, ethical, medical, and patient-centric (Amann et al., 2020). The stakes are especially high in the healthcare industry because mistakes or malfunctions can have a direct effect on people's lives.
One of the paramount issues is the question of liability when AI systems are involved in treatment errors or adverse events. This is complex, given the interrelated technical, organizational and ethical aspects of AI deployment in the health sector (Amann et al., 2020). In addition, Lupton (2018) highlights the importance of developing and upholding ethical and moral structures to shape the development and application of AI so that the benefits of AI are realized responsibly and equitably across society.
Analysis and Findings
Literature has proven that AI significantly transforms the healthcare sector in terms of clinical accuracy, operational efficiency, and environmental security. AI-powered diagnostic tools, particularly for medical imaging, improve sensitivity while reducing false positives and unnecessary procedures. Automating administrative duties also reduces the administrative load on clinicians, freeing time for patient care and generating substantial cost savings.
Telemedicine or Remote diagnostics is also another factor that makes it acceptable and cost-effective for sustaining healthcare. It indirectly benefits the environment and provides an access point, especially for the underprivileged rural population. It aligns with the SDGs and contributes to equity and to intersectoral collaboration for achieving better health among nations.
Yet, ethical issues are pivotal. AI suffers from bias, as in the case where AI based on healthcare data was shown to underestimate health concerns of marginalized groups. Thus, human oversight and transparency in AI’s role are essential to maintaining patient trust and ensuring ethical use. Additionally, environmental sustainability must be considered when optimizing AI’s energy use.Emerging regulations, such as the European AI Act and the European Health Data Space, create guidelines for responsible, understandable, and non-discriminatory AI implementation.
Research Gap
In this fast-growing AI in the healthcare landscape, many research gaps can be outlined, particularly at the intersection between AI, sustainability and marketing. Only a few papers investigated how AI is contributing to sustainable healthcare marketing. Yet, limited research has been conducted on the strategic use of AI to promote environmentally sustainable and ethically sound marketing efforts, even if there is compelling evidence of the efficiencies gained in AI in the realm of medical diagnoses and operations and logistics. This is a vast chasm in our knowledge of how AI can improve efficiency and sustainability in healthcare communication.
Another significant gap is the lack of longitudinal studies examining the lasting impact of AI-fueled healthcare marketing on patient trust, behavioural outcomes, and health. Most existing research focuses on short-term adoption metrics or campaign performance without evaluating how AI influences patient perceptions or decision-making over time. Understanding whether AI enhances or erodes trust in healthcare communications and how this evolves requires more sustained and empirical investigation.
Finally, an extensively documented problem with the under-representation of diverse users in AI training datasets is a significant challenge to fairness and performance. Data that AI systems in health care are trained on often skews in favor of specific demographics, excluding racial, ethnic, linguistic and socioeconomic diversity. This is unethical and detracts from the direct extrapolation and fairness of AI marketing. To ensure the ability to reach out for healthcare services to all cultural groups and to have models that can perform across different cultures, future studies are warranted to validate models on models trained with diverse and representative data.
Conclusion
AI in health is improving diagnosis and patient throughput with sustainability benefits. The inclusion of the technology would allow global health targets, such as the United Nations' Sustainable Development Goals, to ensure more patients can receive care cost-efficiently. However, emerging ethical issues, such as bias, transparency, and privacy, must be reassured that AI works equitably for everyone. There's still an essential human element to maintain trust and medical standards. New regulatory frameworks, including the European AI Act and the European Health Data Space, paved the way for responsible AI regulation. An innovation-with-protection ethos will be a prerequisite for AI to produce the transformation in health care we all hope for. This will open the doors to more dynamic, inclusive and sustainable healthcare systems that serve present and future generations.
References
Ahn, J. S., Shin, S., & Yang, S.-A. (2023). Artificial intelligence in breast cancer diagnosis and personalized medicine. In National Library of Medicine.
Amann, J., Blasimme, A., Vayena, E., Frey, D., Madai, V.I.: Explainability for artificial intelligencein healthcare: a multidisciplinary perspective. BMC Med. Inform. Decis. Mak. 20(1), 1–9(2020).
Ammi, C., Kondrateva, G., & Baudier, P. (2024). Healthcare sustainability: the role of Artificial Intelligence acceptance by medical staff. Journal of Innovation Economics & Management, 44(2), 53-86.
Indexed at, Google Scholar, Cross Ref
Bajwa, J., Munir, U., Nori, A., & Williams, B. (2021). Artificial intelligence in healthcare: transforming the practice of medicine. Future Healthcare Journal, 8(2), e188–e194.
Indexed at, Google Scholar, Cross Ref
Bhatia, A., Guruprasad, M., Basu, C., & Anagh Pathak. (2023). Sustainable Innovations And Impact Of Artificial Intelligence (Ai) In The Indian Healthcare Industry. In Korea Review Of International Studies (Vol. 16, Issue Special Issue 06, pp. 127–129). https://universalai.in/wp-content/uploads/2020/03/Sustainable-Innovations-And-Impact-Of-Artificial-Intelligence-Ai-In-The-Indian-Healthcare-Industry-Kri160623.pdf
Egert, R. (2024). Ethical Considerations for AI use in healthcare marketing. EVERSANA INTOUCH. https://www.eversanaintouch.com/blog/artificial-intelligence/ethical-considerations-for-ai-use-in-healthcare-marketing/
Eiropean Commision. (2025). Artificial intelligence in healthcare. Public Health. Retrieved June 1, 2025, from https://health.ec.europa.eu/ehealth-digital-health-and-care/artificial-intelligence-healthcare_en
Guo, J., & Li, B. (2018). The application of medical artificial intelligence technology in rural areas of developing countries. Health equity, 2(1), 174-181.
Indexed at, Google Scholar, Cross Ref
Lee, D., & Yoon, S. N. (2021). Application of artificial intelligence-based technologies in the healthcare industry: Opportunities and challenges. International journal of environmental research and public health, 18(1), 271.
Safavi, K., & Kalis, B. (2019). How AI can change the future of health care. Harv. Bus. Rev.
Sajwani, R.A. (2024). Artificial_Intelligence_for_Sustainability_Development_in_Healthcare.
SEARO. (2017). Introduction to the Sustainable Development Goals (SDGs). In Background Paper for the Regional Technical Consultation on: Monitoring the Health-Related Sustainable Development Goals (SDGs). https://cdn.who.int/media/docs/default-source/searo/hsd/hwf/01-monitoring-the-health-related-sdgs-background-paper.pdf?sfvrsn=3417607a_4&download=true#:~:text=The%20health%20goal%20(SDG%203,access%20to%20quality%20health%20care.
Thomas, Dr. L. (2024). Ensuring sustainable and responsible use of AI in healthcare. News-Medical. Retrieved June 1, 2025, from https://www.news-medical.net/news/20240805/Ensuring-sustainable-and-responsible-use-of-AI-in-healthcare.aspx
Vinuesa, R., Azizpour, H., Leite, I., Balaam, M., Dignum, V., Domisch, S., & Fuso Nerini, F. (2020). The role of artificial intelligence in achieving the Sustainable Development Goals. Nature communications, 11(1), 233.
Indexed at, Google Scholar, Cross Ref
Received: 10-Jun-2025, Manuscript No. AMSJ-25-15994; Editor assigned: 11-Jun-2025, PreQC No. AMSJ-25-15994(PQ); Reviewed: 18- Jun-2025, QC No. AMSJ-25-15994; Revised: 10-Jul-2025, Manuscript No. AMSJ-25-15994(R); Published: 15-Jul-2025