Review Article: 2022 Vol: 26 Issue: 1
Rejuvenating Dart and Value Co-Creation In Technology Era for Sustainable Healthcare
Vaidik Bhatt, ICFAI Business School (IBS), IFHE University
Samyadip Chakraborty, ICFAI Business School (IBS), IFHE University
Citation Information: Bhatt, V., & Chakraborty, S. (2022). Rejuvenating dart and value co-creation in technology era for sustainable healthcare. Academy of Marketing Studies Journal, 26(1), 1-9.
Abstract
The study describes the value co-creation process in healthcare through the technological advances. Study rejuvenates the popular DART model of value co-creation and extends it by adding a new construct as technology adoption in healthcare disrupted the traditional way of care delivery process. The theoretical study develops the scales using Q sort method and proposes that in the context of business to customer (patients here) the mix of service dominant logic and customer dominant logic enables value co-creation in the healthcare settings. The study enables the understanding regarding the sustainable healthcare and propose the theoretical understanding. The future scope of the study lies in the converting the propositions into testable hypotheses and validate it with large scale data collection.
Keywords
Healthcare; Sustainable Healthcare; DART; Technology Management; Service Dominant Logic; Customer Dominant Logic.
Introduction
In recent years, all sectors have embraced technology developments to harness external resources and skills to create customer centred contact and co-creation of value. Today's healthcare sector is turning to the patient as a co-creator of the offers using current and creative technologies like Internet of Medical Things (IoMT) (Bhatt et al., 2020; Chakraborty et al., 2020), mHealth (Bhatt et al., 2020), and telehealth services (Chakraborty et al., 2018). The use of ICT in healthcare allows patients to transact at any time and location. Patients may now not only access their preferred doctors through mobile health apps, but also monitor their vitals including body temperature, heart rate, blood pressure, and oxygen level (Alam et al., 2019; Talukder et al., 2020). Physicians may easily access patient data through wearable IoMT devices, allowing them to provide comprehensive treatment rather than cure. Telemedicine and mHealth apps enables clinicians to offer care in distant rural areas, meeting community healthcare requirements. Technology has not only improved the patient-physician interaction, but also the bridged the gap of service difference between rural and urban areas (Srivastava & Shainesh, 2015).
With the current paradigm change in healthcare, merely treating sickness is no longer crucial. Hospitals, nurses, physicians, beds, ambulatory services, medical gadgets, etc. are examples of things that do not contain inherent value alone (Joiner & Lusch, 2016). With rising healthcare costs and technological breakthroughs, people' expectations have risen. Patients want more than just preventative and acute care from their healthcare providers. Patients desire to be more involved in decision making (Bhatt & Chakraborty, 2021b, 2021a). Patients are seen as co-creators of healthcare services. Patients want providers and healthcare organisations to be part of their everyday routine, thus healthcare organisations should look at patients' ecosystems and realities.
Many research show the value of co-creation. In the B2B (Business to Business) scenario, where focal firm gains a competitive advantage via co-creation activities with downstream and upstream network actors (Chakraborty, 2018; Mazur & Zaborek, 2014; Prahalad & Ramaswamy, n.d., 2004; Taghizadeh et al., 2016). However, these study fails to cover end consumers’ point of view and involvement as a co-creator. In this age of technology breakthroughs and shifting consumer perspectives, the patient is a co-creator of the healthcare service (Seppänen et al., 2017), and patients’ view needs to be covered when providers are seeing the patient as a value co-creator in service delivery process.
The spread of new healthcare technology exposes several flaws in the DART framework. The traditional DART paradigm (Prahalad & Ramaswamy, 2004) focuses on value co-creation between upstream and downstream supply chain stakeholders, ignoring end customers. However, in an age of technological breakouts, when the healthcare business is seeing significant shifts in market dynamics, it is critical to include patients viewpoint.
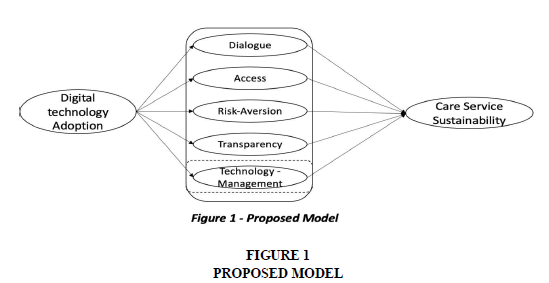
The study's goal is to build DARTT a DART framework with a fifth dimension: technology management (dialogue, Access, Risk Aversion, Transparency, Technology Management). We believe that the standard DART paradigm assumes that modern healthcare technology is only used to communicate with stakeholders. However, the study attempts to analyse how technology management helps patient co-creation of health care services. The study finds it intriguing that provider-side technology management helps patients co-create service value.
Conceptual Background
Theoretical Underpinnings
S-D Logic highlights the network partners' value co-creation process. Unlike classic good dominance reasoning, S-D Logic sees value in network actors co-creating service (Lusch & Vargo, 2011; Vargo & Lusch, 2008). With the beneficiary as a resource integrator, S-D Logic asserts that value is always co-created by integration of various network actors (Vargo & Lusch, 2016). This altered the conventional co-production of services and dietic connections. However, S-D Logic asserts that the value is always set by the end user, not the network actors, and that the network actors operate as resource integrators and they provide value proposition only. However, in silos, they have no fundamental worth. As stated by (Joiner & Lusch, 2016), patients cannot co-create or define value with physical resources such as network actors such as physicians, nurses, pharmacies, hospital beds, and infrastructure. As resource integrators, they assists to co-create value. S-D Logic states that network partners produce value together (Edvardsson et al., 2011; Lusch et al., 2007; Vargo & Akaka, 2009; Vargo & Lusch, 2017).
Aside from the classic B2B context and the newer idea of B2C services, SDL does not look at the customers' eco-system and routine. It starts with the customer's routine, where the supplier is engaged in their everyday life (Heinonen et al., 2010; Heinonen & Strandvik, 2015). In recent times, it is critical to comprehend the customer's viewpoint. Because patients are a specific sort of client in healthcare, it is critical to understand their reality and everyday life in order to give care. While SDL focuses on value co-creation, with the end user as a co-creator, CDL focuses on value in usage. In SDL, the service provider controls the service process and interactions, whereas in CDL, the customer defines the value. Instead than focusing on interactions and co-creation, CDL sees service delivery as adding value to consumers' lives (Heinonen et al., 2010; Heinonen & Strandvik, 2015; Seppänen et al., 2017).
Digital Technology Adoption
The innovation in information and technology domain does not only enhanced the standards of living but also enhanced expectancy of life also. Although the healthcare sector is far behind in adopting the innovative technology, the pandemic of covid-19 worked as a catalyst for healthcare to adopt the technology. During the lockdown and border closure when the people were afraid of going outside, due to the risk of infection form covid-19, various technologies have helped them to fulfil their healthcare needs (Bhatt et al., 2020). People has started to use the wearables and mHealth to be in touch with their family physician or the physician of their choice for the people of various chronic disorders, whereas mHealth apps also used for the consulting a physician for acute diseases. Telemedicine has been used widely in the covid-19 period for satisfying the healthcare needs of the rural area using hub and spoke model(Bhatt et al., 2020; Chakraborty et al., 2018; Chandwani et al., 2018).
The technology provides a platform for interaction between the patient-patient, patient-physician and physician and other healthcare network actors (Osei-Frimpong et al., 2018). However this interaction should be deep and frequent (Autry et al., 2014). The digital technology adoption by patient, provider and other network actors in a healthcare sector enables them to frequent connect with each other and share their view points. Also, it provides a real-time and accurate access regarding the patients’ vitals to physician (Bhatt & Chakraborty, 2021c, 2020; Zamanifar, 2021), by which physician can take care of the patients using predictive modelling and analyse the future risks (Bhatt et al., 2022). On the other end, patients can also have an access to the medical facilities through telemedicine centres in rural area and mHealth apps in urban and semi urban area, where irrespective of time and place they can interact with the physicians and assess the risk by their experience, star ratings and other details to make an informed decision while selecting the doctor (Bhatt & Chakraborty, 2021b; Osei-Frimpong et al., 2018). The interaction and communication is successful only if the transparent exchange of knowledge and information is there (Taghizadeh et al., 2016). Interaction without transparency is worthless as trusts between the network actors is important. Digital technology adoption leads towards the real-time and transparent exchange of information and knowledge between the network actors (Bhatt & Chakraborty, 2020; Chakraborty et al., 2021). However, despite of the technological advances and technological adoption, it does not create any value, as technologies like mHealth, telemedicine, IoMT ete provides value propositions only, as it cannot create the value in space, but it is about how one manages the technology and uses own capability to exploit the technology which creates the final outcome as value (Bharadwaj, 2000; Zhang et al., 2008). However, for technology adoption is a precursor / primary stage to mage the technology. Here it is proposed that,
Proposition 1: Level of digital technology adoption is positively related to the level of dialogue
Proposition 2: Level of digital technology adoption is positively related to the level of access
Proposition 3: Level of digital technology adoption is positively related to the level of risk assessment
Proposition 4: Level of digital technology adoption is positively related to the level of transparency
Proposition 6: Level of digital technology adoption is positively related to the level of technology management
DART
Traditionally DART was conceptualized with a view for providing the building blocks for value co-creation, with high quality interactions and information sharing between the network partners (Prahalad & Ramaswamy, 2004). The locus of value co-creation is between the company and customer, where service provider will not always controls the process, but involves in the customers’ life and provide the offerings which creates the value for the customers. Here, co-creation cannot be seen as an outsourcing activity for the firm, but it’s about the involvement of company into customers’ life and involvement of customers in company’s operations (Heinonen et al., 2010).
Traditional building blocks of dialogue, access, risk aversion and transparency seems to be the satisfactory elements to understand the value co-creation activity at the first sight (Chakraborty, 2018, 2019; Taghizadeh et al., 2016) . It seems to be perfect for driving the interactions and to reduce the potential risk of asymmetry in data (Albinsson et al., 2016). However, it does not through the light on using the technology infrastructure as asset for sustainable ubiquitous healthcare framework where technology is not only used for the enhancing communication, dialogue and reducing the data asymmetry. In the recent technological era, physician cannot only control the co-creation of the service as described in S-D Logic, but also enabled to look into the patients’ ecosystem, routine and habits with wearable health devices (Bhatt & Chakraborty, 2021b, 2021a), and mHealth apps (Khatun et al., 2015). On the other end, patients are also empowered enough to check the doctors’ ratings given by other patients, location, qualification, experience etc. which helps then to take an informed decision while selecting the physician for the treatment (Aamir et al., 2018; Alam et al., 2020). In this context, using the technological infrastructure merely for communication won’t provide competitive edge. mHealth and IoMT devices acts as more than the infrastructure for the dialogue, access and transparency. Patients are empowered to co-create their experiences with the different manner, with different types of interactive processes and personalize their experiences. In the recent context, technology management is important and the study is looking to extend the existing DART framework by inclusion of Technology Management Figure 1.
In recent times, hospitals have become the small part of the larger healthcare ecosystem (Digital Health Ecosystems: A Payer Perspective McKinsey, n.d.), where hospitals interacts with different bodies like telemedicine centre, primary health centres, ambulatory centres, pathology and radiology labs, pharmacy etc, to provide a holistic care to the patient. World is leading towards building the sustainable society, and a healthcare is one of the primary pillars for it. For building a sustainable healthcare, it is important that people of every segment and demographics should get an affordable and ubiquitous access to the quality healthcare (Chakraborty & Bhatt, 2020). For providing sustainable healthcare, healthcare ecosystem should be enabled enough to have a dialogue with network partners, to have an access towards that each other’s’ data, should able to assess the risks with each other and with the patients in a transparent manner (Chakraborty, 2018, 2019). Also, network actors should be able to manage the technology properly for generating the value for themselves and for patients (Zhang et al., 2008). The study proposes that,
Proposition 6: Level of dialogue between network actors is positively related to the sustainable healthcare
Proposition 7: Level of access between network actors is positively related to the sustainable healthcare
Proposition 8: Level of risk-assessment between network actors is positively related to the sustainable healthcare
Proposition 9: Level of transparency between network actors is positively related to the sustainable healthcare
Proposition 10: Level of technology management between network actors is positively related to the sustainable healthcare
Research Methodology
The primary objective of the study is to rejuvenating the DART model (Prahalad & Ramaswamy, 2004) in the today’s context of technological advancement which helps in formation of sustainable society with sustainable and equitable healthcare as a primary pillar. A rigorous literature review has been performed on digital technology adoption, sustainable healthcare, DART framework and co-creation literature in a first step. The extensive literature review helped in developing the relationships between the constructs, it also helped in generation of pool of items for a scale development. The definitions have been adapted from different literature for different constructs and pool of items generated. The initial pool of items were validated by four academicians having research at the integration of service marketing, service delivery and healthcare technology adoption. They have been asked to check and validate the face validity of constructs by matching the definitions and pool of items generated. In the third stage, the study follows method of Q sort (Moore & Benbasat, 1991) for generating the final measurement scales. This method has been widely used for the scale development study, where researchers’ needs to adapt the pool of items as per the defined constructs (Bhatt et al. 2019, 2020; Chakraborty et al. 2020). In the third stage for checking the convergent and discriminant validity for the constructs, three academicians and three industry experts were invited having experience at the intersection of healthcare, technology and services. After the three rounds of Q sort, the study reaches to the mutual consent form the six experts regarding measurement items. The study uses inter-rater reliability, raw agreement score and cohen’s kappa for finalizing the measurement items. At the end of the third round, we found that all these scores are above 0.9, which is the satisfactory condition for a scale development process by Q sort method.
Results and Discussion
As a result of Q sort method, the study developed the measurement scales for the constructs. After the three rounds of omitting the items one by one the study founds final measurement scales as hit ratio, inter-rater reliability and conhen’s kappa were found to be more then 0.90. which is a satisfactory contrition for scale development using Q Sort method. The final measurement items along with the adapted definitions of the constructs provided in the Table 1 below.
| Table 1 Measurement Items As A Result Of Q Sort Method |
||
|---|---|---|
| Construct | Items | References |
| Digital technology Adoption | Healthcare network actors are documenting patients’ records in the digital format Healthcare network actors successfully converts the medical reports to the electronic and analysable format Healthcare network actors uses the digitized technology for viewing health report, diagnostics data and laboratory reports Healthcare network actors are successfully capturing the medication prescription given to the patient in digital and sharable format |
(Bhatt et al., 2020; Bhatt & Chakraborty, 2021b) |
| Dialogue | Network actors has frequent communication with each other on a regular basis Network actors have opened their doors for two way communication Network actors have informal and formal communication Network actors involve internal and external parties while communicating with each other |
(Chakraborty, 2019; Taghizadeh et al., 2016) |
| Access | Network actors shares timely information with each other Network actors provides real-time information with each other Network actors provides an opportunity to each other for service development Network actors clearly states their requirements with each other Network actors emphasize more on service experience rather than ownership of the product |
(Chakraborty, 2018, 2019; Taghizadeh et al., 2016) |
| Risk-Assessment | Network actors are sharing potential risks with each other Provider shares potential risks with the patient and vice versa Network actors informs each other regarding their own constraints Network actors shares all responsibilities related to the risk with each other |
(Albinsson et al., 2016; Chakraborty, 2019; Taghizadeh et al., 2016) |
| Transparency | Network actors clearly explains their requirements with each other Network actors shares accurate information with each other Network actors shares all the required information with each other Network actors does not hide any vital information with each other for personal benefits |
(Albinsson et al., 2016; Chakraborty, 2018; Taghizadeh et al., 2016) |
| Technology management | Network actors have integrated IT applications with each other Network actors have clarity about how technology provides value to each other Network actors have installed devices for remote database access Network actors uses IT based collaborations Network actors developed technology based integration links with each other |
(Bharadwaj, 2000; Zhang et al., 2008) |
| Care Service Sustainability | Healthcare system is able to provide timely care services to the patients Healthcare system is able to provide care services to the remote interior area Healthcare system is able to fulfil healthcare needs of surrounding communities Healthcare system is able to provide care to all the patients |
Newly Created in the context of the study |
Conclusion and Implication
The study highlighted a new notion of developing a sustainable and equitable healthcare by extending the DART paradigm of value co-creation given by (Prahalad & Ramaswamy, 2004). In the technological era, where every work is technology oriented, it is important to manage the technology, however the traditional DART model, does not includes the role of technology for value co-creation. There are various studies done on traditional DART model (Chakraborty, 2018, 2019; Taghizadeh et al., 2016), however, any of these studies does not include the role of the technology in value co-creation process. However, we believe that, technology plays a primary role and provides the basis for dialogue, access and transparency. On the other end, technology provides an opportunity to access the risks with the real-time and accurate data sharing capabilities.
The study contributes to the academic literature by breaking the notion of service dominant logic. Most of the previous studies on DART and co-creation has been performed in the B2B context, where customers’ view point was not captured in the co-creation process, only viewpoint from the company side was captured (Chakraborty, 2018, 2019; Taghizadeh et al., 2016). In this business to business context service dominant logic may show its dominance for the business transactions, however, it fails to provide understanding about the end consumers’ view point (Heinonen et al., 2010; Heinonen & Strandvik, 2015). This study takes in to consideration of both the logics as CD logic (Heinonen et al., 2010) as well as SD logic (Lusch & Vargo, 2011; Vargo & Lusch, 2008), and concludes that in healthcare context any one of the logics in silos will not work. However, healthcare sector will work on the mix of both the logics to provide a holistic care to society. The study also emphasize the role of patient as co-creator and other healthcare network actors like mHealth providers, telemedicine centres, ambulatory centres etc. as they are the integral part of the healthcare system which helps in providing equitable care services to the all the segments of society and thereby helping a world to move towards sustainability.
Limitations and Future Scope
This study is one of the first study performed towards making a sustainable and equitable healthcare for all the segment of society using digital technology adoption at various levels and also breaks the notion of DART framework by extending it. The study also breaks the traditional notion of B2B study for the co-creation and add the B2C view point also in the context of healthcare services to the literature. However, the study has some limitations. This study is theoretical study only which provides measurement scale development process through Q sort method. The study lacks in generating empirical evidences form the large scale data collection. The future scope also lies in the converting the propositions in to testable hypotheses for collecting the large scale data and validate the claims made by the theoretical understanding.
References
Aamir, J., Ali, S.M., Kamel Boulos, M.N., Anjum, N., & Ishaq, M. (2018). Enablers and inhibitors: A review of the situation regarding mHealth adoption in low- and middle-income countries. Health Policy and Technology, 7(1), 88–97.
Bharadwaj, A.S. (2000). A RESOURCE-BASED PERSPECTIVE ON INFORMATION TECHNOLOGY CAPABILITY AND FIRM PERFORMANCE: AN EMPIRICAL INVESTIGATION 1. In Bharadwaj/IT Capability and Firm Performance MIS Quarterly 24, 1.
Bhatt, V., Chakraborty, S., & Chakravorty, T. (2020). Importance of Digitech Adoption for Providing Efficient Healthcare Services during COVID-19. International Journal on Emerging Technologies, 11(3), 1–13.
Digital health ecosystems: A payer perspective | McKinsey. (n.d.). Retrieved April 22, 2020, from https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/digital-health-ecosystems-a-payer-perspective
Osei-Frimpong, K., Wilson, A., & Lemke, F. (2018). Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technological Forecasting and Social Change, 126, 14–27. https://doi.org/10.1016/j.techfore.2016.04.009
Taghizadeh, S.K., Jayaraman, K., Ismail, I., & Rahman, S.A. (2016). Scale development and validation for DART model of value co-creation process on innovation strategy. Journal of Business and Industrial Marketing, 31(1), 24–35.